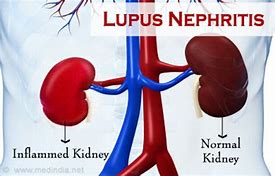
I’ve just discovered that a family member has lupus nephritis. I need to remind myself what that encompasses. Looks like you’re coming on this quest with me this week. Just in case you’ve forgotten what lupus nephritis is, Doctors Health Press is here to help us out:
“Lupus Nephritis
Lupus nephritis is inflammation of kidneys caused by the autoimmune disease known as systemic lupus erythematous (SLE)—also called lupus. This is where the body’s immune system targets its own tissues.
As many as 60% of lupus patients will later get lupus nephritis. The most common symptoms include dark urine, weight gain, high blood pressure, foamy urine, and the need for nighttime urination.”
I turned to Tampa General Hospital for more information:
““Nephritis causes one or both kidneys to become inflamed and leak protein into the urine.
Nephritis is an inflammation of the kidneys. These important organs clean the blood by filtering out excess fluid and toxins, then eliminate those waste products from the body in the form of urine. Healthy kidneys do not remove proteins from the blood, which help the body absorb water. However, inflamed kidneys can leak protein into the urine, which can impair the body’s ability to absorb water and lead to tissue swelling.”

I figured the National Kidney Foundation would be the likeliest place to find the treatment for lupus nephritis [and it was, sort of]:
- “Corticosteroids (often called ‘steroids’)
- Immunosuppressive drugs
- Monoclonal antibodies
- ACE inhibitors and ARBs
- Diuretics
- Diet change”
Sort of? you ask. This has been the usual treatment plan, but there’s been an advancement. Yale Medicine explains:
“… the introduction of the two new therapies approved in 2021 that are specifically targeted for lupus. While older medications have been designed to suppress the body’s entire immune system, these new drugs target specific molecules.
There are now three of these targeted medications:
- Saphnelo (anifrolumab)—approved in August 2021. This monoclonal antibody (a protein that finds and attaches to one type of substance, called a cytokine, in the body) is designed to treat an excess of interferon activation, which plays an essential role in lupus inflammation. It’s administered by intravenous infusion.
- Benlysta (belimumab)—approved in 2011, is also a monoclonal antibody; it targets a protein that may help lessen the impact of abnormal cells that contribute to inflammation in lupus. It’s given by injection in the abdomen or thigh—or by intravenous infusion. It is approved for use in children ages 5 and older, and was recently approved in 2020 for adults who have lupus with kidney involvement.
- Lupkynis (voclosporin)—approved in January 2021, is the first oral medication FDA-approved for lupus nephritis. It works by helping to stop cells that cause inflammation in lupus nephritis, while protecting the kidneys from serious damage….
But it is the targeted treatments that could ‘move the needle’ on helping more patients reach remission, Dr. Koumpouras explains. With the three most recent medications, ‘we’ve [stet] actually improved the treatment outcomes for patients with SLE,’ he says. ‘We know that, statistically, patients will do better on these treatments.’”
Dr. Koumpouras is “Fotios Koumpouras, MD, director of the Yale Lupus Program, which provides a comprehensive evaluation of and treatment to lupus patients. It also offers programs, such as a combined rheumatology-dermatology clinic (the first of its kind in Connecticut), and access to clinical trials.”
We know any drug may have side effects. Following are those for these two new and one not so new treatments for lupus nephritis:
Daily Med for Saphnelo –
“The following side effects may get better over time as your body gets used to the medication. Let your healthcare provider know immediately if you continue to experience these symptoms or if they worsen over time.

Common Side Effects
- Upper respiratory infection (34%)
- Bronchitis (11%)
- Infusion-related reactions (headache, dizziness, nausea; 9%)
- Herpes zoster infection (shingles; 6%)
- Cough (5%)
Other Side Effects
- Other respiratory infections
- Allergic reactions
Serious Side Effects
Contact your healthcare provider immediately if you experience any of the following.
- Severe infection: confusion, fever, difficulty breathing, weakness, cough, sweating, chills, stomach pain, diarrhea, burning sensation when you urinate
- Serious allergic reaction (anaphylaxis): difficulty breathing, tightness in the throat, hives, itching, fast heartbeat, nausea, dizziness, lightheadedness, swelling in the face or tongue“
Benlysta for Benlysta –
Infections
Infections could be serious, leading to hospitalization or death. Tell your healthcare provider right away if you have any of the following symptoms of infection: fever, chills, pain or burning with urination, urinating often, coughing up mucus, or warm, red, or painful skin or sores on your body.
Allergic (hypersensitivity) reactions
Serious allergic reactions can happen on the day of, or in the days after, receiving BENLYSTA and may cause death. Your healthcare provider will watch you closely while you are receiving BENLYSTA given in a vein (intravenous infusion) and after your infusion for signs of a reaction. Allergic reactions can sometimes be delayed. Tell your healthcare provider right away if you have any of the following symptoms of an allergic reaction following use of BENLYSTA: itching, swelling of the face, lips, mouth, tongue, or throat, trouble breathing, anxiousness, low blood pressure, dizziness or fainting, headache, nausea, or skin rash.
Mental health problems and suicide
Symptoms of mental health problems can occur. Tell your healthcare provider right away if you have any of the following symptoms: thoughts of suicide or dying, attempt to commit suicide, trouble sleeping (insomnia), new or worse anxiety, new or worse depression, acting on dangerous impulses, other unusual changes in your behavior or mood, or thoughts of hurting yourself or others.”
WebMD for Lupkynis –
“Headache, tiredness, dizziness, diarrhea, shaking, upset stomach, or abdominal pain may occur. If any of these effects last or get worse, tell your doctor or pharmacist promptly.
Temporary hair loss may occur. Normal hair growth should return after treatment has ended.
People using this medication may have serious side effects. However, you have been prescribed this drug because your doctor has judged that the benefit to you is greater than the risk of side effects. Careful monitoring by your doctor may decrease your risk.
This medication may raise your blood pressure. Check your blood pressure regularly and tell your doctor if the results are high. Your doctor may control your blood pressure with medication.”
Tell your doctor right away if you have any serious side effects, including: signs of kidney problems (such as a change in the amount of urine), mental/mood changes (such as confusion, changes in alertness), easy bruising/bleeding, numbness/tingling, vision changes.
Get medical help right away if you have any very serious side effects, including: seizures.
A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.”
This is neither meant to scare you or insinuate that you will experience these side effects. Your doctor will keep an eye on you to see if you develop any of these side effects. You need to keep an eye on you, too.
Until next week,
Keep living your life!



How about “lupus – like “ nephritis. ?
<
div>I have th
The best I could figure out is what The National Library of Medicine has to offer: “patients without overt systemic lupus erythematosus (SLE) present with biopsy findings typically seen in lupus nephritis (LN). Although a minority eventually develops SLE, many do not. It remains unclear how to classify or treat these patients.” Whatcheer, please speak with your nephrologist about this.