Hello, hello, and a belated welcome to National Kidney Month. This year, for a change, I decided to go to a non-medical site for a clear explanation of what this month is. The entire blog [except my introduction, of course.] is from National Today, a site committed to which celebrations are on which day[s]:
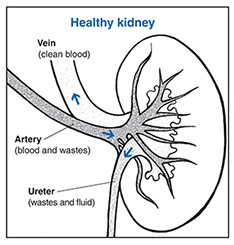
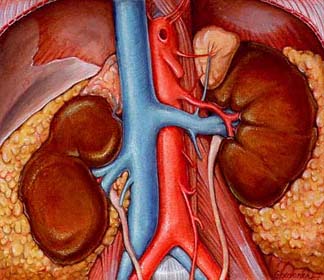
“March is dedicated to National Kidney Month. The kidneys, two bean-shaped organs located in the back of the abdomen, perform crucial functions to filter out toxins, produce red blood cells, and regulate pH. They filter about half a cup of blood every hour, creating urine from harmful and unnecessary waste.
When kidneys fail to function properly, waste builds up in the blood and leads to a weakened system and a host of problems like anemia, nerve damage, and high blood pressure. Chronic kidney disease(CKD) affects more than 1 in 7 American adults and is the 9th leading cause of death in the U.S.
HISTORY OF NATIONAL KIDNEY MONTH
National Kidney Month, observed every March, brings awareness to kidney health and encourages people to support kidney disease research and take steps to keep their own kidneys safe and healthy.
Kidneys filter blood, make urine, and produce the red blood cells that carry oxygen through your body. These vital organs also control blood pressure and produce vitamin D to keep bones strong.
Malfunctioning kidneys can lead to painful kidney stones and infections that, left untreated, require a transplant. Some pre-existing conditions, like high blood pressure and diabetes, put you at increased risk for kidney disease.
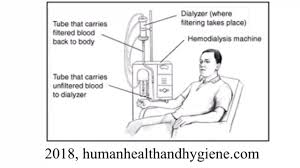
Chronic Kidney Disease(CKD) affects almost 40 million American adults. In 2016, three-quarters of a million people in the U.S. required dialysis or a kidney transplant. Dialysis and kidney transplants, the only treatment options for severe kidney failure, are difficult, expensive, and not always available. Patients seeking new organs may not always get them in time to survive; in the U.S., twelve people die each day waiting for a kidney.
To prevent kidney disease, the National Kidney Foundation recommends taking proactive steps to keep your kidneys healthy and prevent the onset of CKD. You can protect your kidneys by managing high blood pressure, making healthy food and drink choices, and reducing stress.
The National Kidney Foundation grew out of a mother’s determination to further research into treatment for kidney conditions. When her infant son was diagnosed with nephrosis, Ada DeBold started the Committee for Nephrosis Research to organize efforts to find treatments and connect patients and doctors. DeBold continued crusading for the organization, which eventually became the National Kidney Foundation. The Foundation conducts fundraising to support important research into the treatment and prevention of kidney disease.
NATIONAL KIDNEY MONTH TIMELINE
1984
National Organ Transplant Act Passes
The NOTA establishes the National Organ Procurement and Transplantation Network, which maintains an organ matching registry to address organ shortages and streamline the donation process.
1954
First Successful Kidney Transplant
The first successful kidney transplant is performed between two identical twins in Boston.
1943
Dialysis Invented
Dutch doctor Willem Kolff invents the ‘artificial kidney’ to clean the blood of kidney failure patients.
1902
Animal Experiments
The first successful kidney transplants in animals are performed at the Vienna Medical School.
NATIONAL KIDNEY MONTH FAQS
What month is National Kidney Month?
National Kidney Month is observed annually during the month of March.
Is there a ribbon for kidney disease?
Kidney Disease Awareness is symbolized by the color green. Purchase green ribbons, green wristbands, or green magnets directly from a Kidney Disease Awareness non profit in order to help raise funds for treatments.

What are the symptoms of chronic kidney disease?
Symptoms include difficulty urinating or less urine, sweeping in the extremities, shortness of breath, nausea, and feeling cold and tired. If you experience chronic symptoms that you suspect are related to kidney function, consult your physician.
HOW TO OBSERVE NATIONAL KIDNEY MONTH
- Join the organ donor registry
Most organ donations come from deceased people. Register to be an organ donor when you die and your healthy organs and tissue can save dozens of lives.
- Donate to a kidney non-profit
Non-profit organizations do the important work of raising awareness about kidney disease, providing resources and assistance to patients, and connecting patients, doctors, and donors.
- Be good to your kidneys
Are you keeping your kidneys healthy? Aim for a lower intake of sodium and sugars, more whole grains and low-fat dairy, and regular exercise to reduce your risk of kidney disease, high blood pressure, diabetes, and other diseases.
5 FASCINATING FACTS ABOUT KIDNEYS
- You only need one kidney to live
Although you’re born with two kidneys, each of which have about 1.5 million blood-filtering units(nephrons), you only need about 300,000 nephrons to filter your blood properly.
- Your kidneys are lopsided
The right kidney is slightly smaller and sits lower than the left to make room for another important organ, the liver.
- You can drink too much water
This can cause a condition called hyponatremia, which, though not common, can damage the kidneys.
- Sausage casing and orange juice cans
Willem Kolff, who invented the first artificial kidney that led to today’s dialysis technology, used sausage casings, orange juice cans, and a washing machine to create a rudimentary blood cleaning mechanism.
- Climate change may increase kidney disease
As parts of the world get warmer, the dehydration that leads to kidney disease is likely to rise among manual laborers.
WHY NATIONAL KIDNEY MONTH IS IMPORTANT
- It reminds us to be good to our bodies
Make sure you take care of your body and your vital internal organs so they can continue taking care of you.
- It’s a chance to express gratitude for our health
If you have fully functional kidneys, be grateful! Take a minute to feel gratitude for all the internal organs that do the invisible, daily work of keeping us alive.
- It shows that science is awesome
Just a few decades ago, kidney disease could mean a death sentence. Today, although it’s still a serious and frightening illness, we can often fight off kidney failure with dialysis and organ transplants.”
Many thanks to National Today for their simple, straight forward explanation of National Kidney Month.
Until next week,
Keep living your life!







































 Why not, you may be asking yourself. Easy answer? I’m allergic to them. Wait just a minute here. What exactly does allergic mean and how will this affect your Chronic Kidney Disease?
Why not, you may be asking yourself. Easy answer? I’m allergic to them. Wait just a minute here. What exactly does allergic mean and how will this affect your Chronic Kidney Disease?
 I’ve satisfied myself that, just as with my food allergies, my sensitivity to lactose, wheat, fructose syrup, and acidic foods will not harm my kidneys. Although, they may cause me to read more food labels than I usually do. Hopefully, you’re satisfied that your food allergies and sensitivities will not harm your kidneys. If you’re still concerned, speak with your nephrologist or renal dietitian.
I’ve satisfied myself that, just as with my food allergies, my sensitivity to lactose, wheat, fructose syrup, and acidic foods will not harm my kidneys. Although, they may cause me to read more food labels than I usually do. Hopefully, you’re satisfied that your food allergies and sensitivities will not harm your kidneys. If you’re still concerned, speak with your nephrologist or renal dietitian.
 Here’s hoping those of you in the U.S.A. had a safe and thoughtful July 4th. This is a peculiar year with different kinds of celebration or none at all.
Here’s hoping those of you in the U.S.A. had a safe and thoughtful July 4th. This is a peculiar year with different kinds of celebration or none at all.

 It seems that most of them are taking lithium to help control the bipolar disorder. Okay, I’ll bite: what is lithium? Drugs.com at
It seems that most of them are taking lithium to help control the bipolar disorder. Okay, I’ll bite: what is lithium? Drugs.com at 
 The most common problem from taking lithium is a form of diabetes due to kidney damage called nephrogenic diabetes insipidus. This type of diabetes is different than diabetes mellitus caused by high blood sugar. In nephrogenic diabetes insipidus, the kidneys cannot respond to anti-diuretic hormone (ADH), a chemical messenger that controls fluid balance. This results in greater than normal urine out-put and excessive thirst. It can be hard to treat nephrogenic diabetes insipidus.”
The most common problem from taking lithium is a form of diabetes due to kidney damage called nephrogenic diabetes insipidus. This type of diabetes is different than diabetes mellitus caused by high blood sugar. In nephrogenic diabetes insipidus, the kidneys cannot respond to anti-diuretic hormone (ADH), a chemical messenger that controls fluid balance. This results in greater than normal urine out-put and excessive thirst. It can be hard to treat nephrogenic diabetes insipidus.”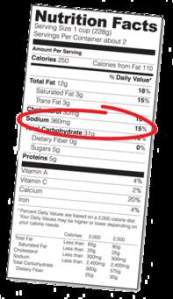
 awareness to those living with (and without) Chronic Kidney Disease.
awareness to those living with (and without) Chronic Kidney Disease.
 husband, who doesn’t have CKD, loved them, too. I enjoyed their pasta products, too. Now, lest you get the wrong idea, I am not endorsing this company because I don’t know what others like it are available. However, I wanted to know about their products… which may very well be similar to the products of other such companies and, therefore, helpful to CKD patients.
husband, who doesn’t have CKD, loved them, too. I enjoyed their pasta products, too. Now, lest you get the wrong idea, I am not endorsing this company because I don’t know what others like it are available. However, I wanted to know about their products… which may very well be similar to the products of other such companies and, therefore, helpful to CKD patients.
 from
from 
 “A chronic inflammatory disease that is caused by autoimmunity. Patients with
“A chronic inflammatory disease that is caused by autoimmunity. Patients with 
 Conservative treatments
Conservative treatments
 I don’t think I’ve ever felt this tired in my life. Cancer does that… and it leaves me a lot of time in bed to explore whatever I’d like to on the internet. So now I’m discovering all these – what’s the word? – possibly peripheral? diseases that affect the kidneys. For example, while I don’t have the energy to post a new Chronic Kidney Disease picture on Instagram every day, I do check the site daily and like what appeals to me and learn from what’s new to me.
I don’t think I’ve ever felt this tired in my life. Cancer does that… and it leaves me a lot of time in bed to explore whatever I’d like to on the internet. So now I’m discovering all these – what’s the word? – possibly peripheral? diseases that affect the kidneys. For example, while I don’t have the energy to post a new Chronic Kidney Disease picture on Instagram every day, I do check the site daily and like what appeals to me and learn from what’s new to me. Hmmm, so kidney disease can cause you to lose too much potassium, which can then interfere with the proper functioning of your kidneys. Doesn’t sound good to me. But, remember that the condition is congenital and will show up at birth.
Hmmm, so kidney disease can cause you to lose too much potassium, which can then interfere with the proper functioning of your kidneys. Doesn’t sound good to me. But, remember that the condition is congenital and will show up at birth. “What foods are high in potassium (greater than 200 milligrams per portion)? The following table lists foods that are high in potassium. The portion size is ½ cup unless otherwise stated. Please be sure to check portion sizes. While all the foods on this list are high in potassium, some are higher than others.
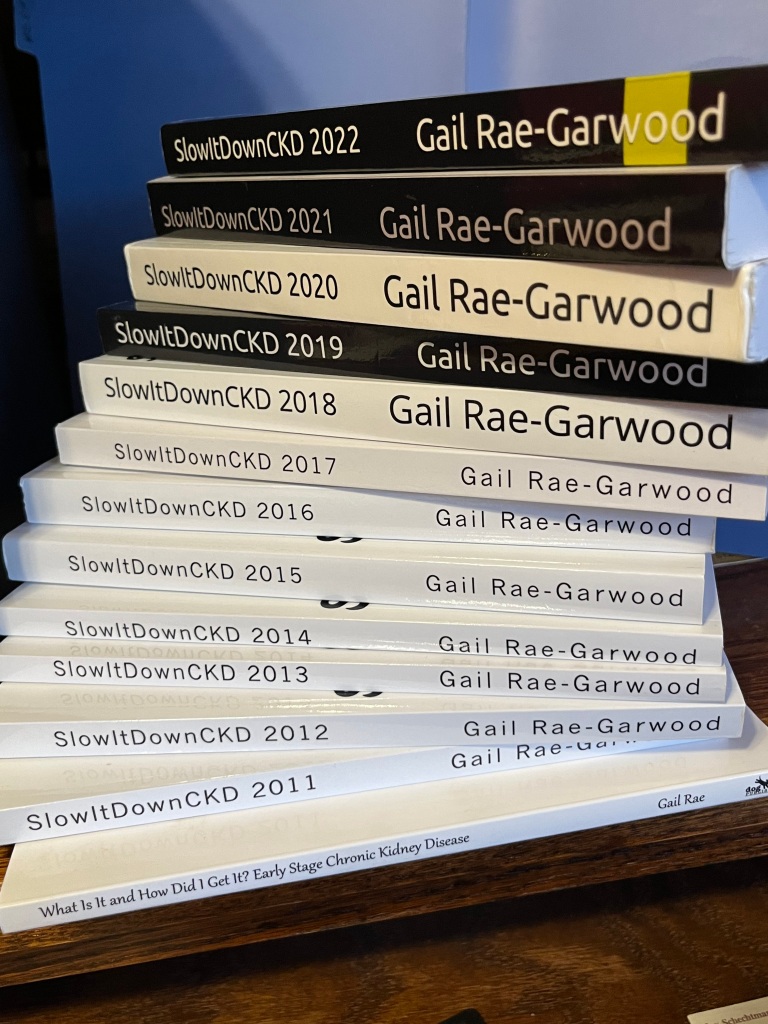
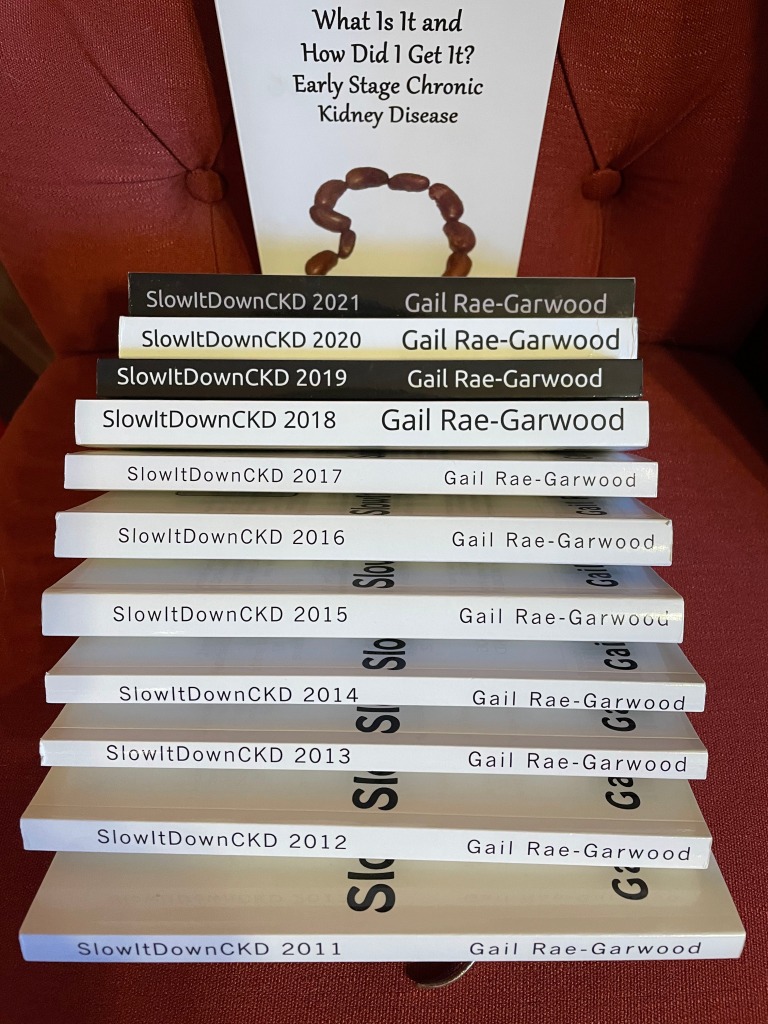
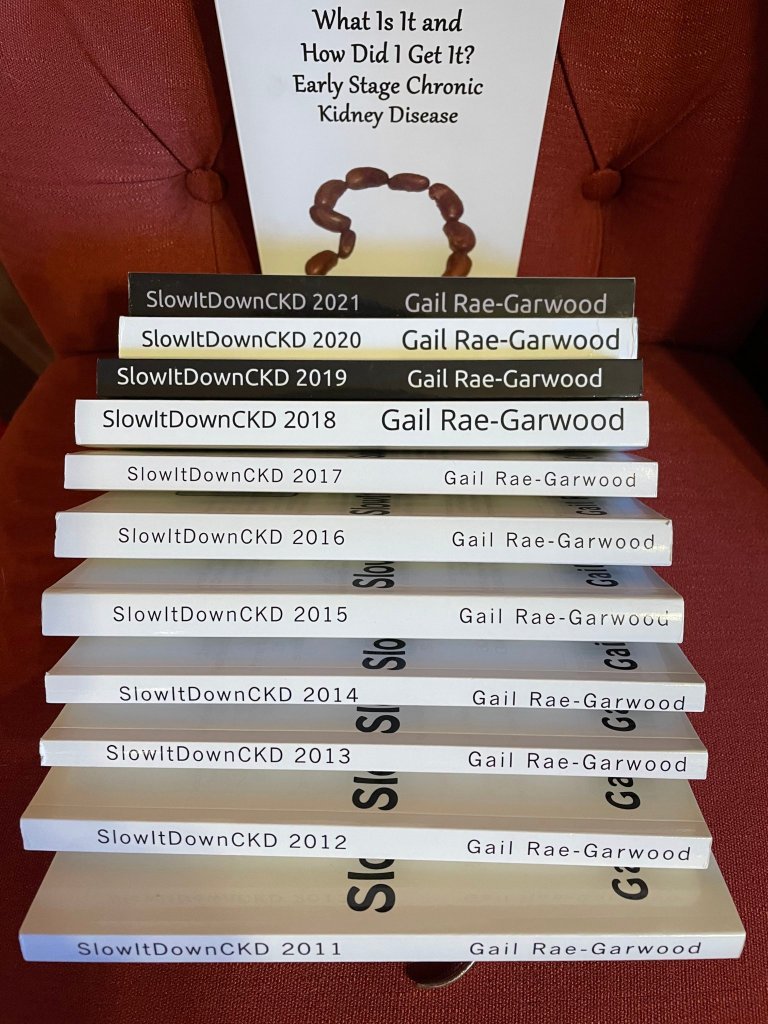
“What foods are high in potassium (greater than 200 milligrams per portion)? The following table lists foods that are high in potassium. The portion size is ½ cup unless otherwise stated. Please be sure to check portion sizes. While all the foods on this list are high in potassium, some are higher than others. I also wanted to remind you that the SlowItDownCKD series makes a wonderful graduation, wedding, and Father’s Day gift for those new to Chronic Kidney Disease, those not new to Chronic Kidney Disease, and those who would like to share CKD with others in their lives.
I also wanted to remind you that the SlowItDownCKD series makes a wonderful graduation, wedding, and Father’s Day gift for those new to Chronic Kidney Disease, those not new to Chronic Kidney Disease, and those who would like to share CKD with others in their lives. Tubules, huh? What are those? Actually, the word just means tube shaped. Remembering that renal and kidney mean the same thing, we can see the problem area.
Tubules, huh? What are those? Actually, the word just means tube shaped. Remembering that renal and kidney mean the same thing, we can see the problem area.

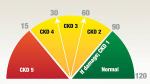
 As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book,
As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book, 
 A GFR of 55 is the higher part of stage 3A. 60 is where stage 2 of CKD begins. My kidneys were functioning better on chemo. And the creatinine? Let’s get a quick definition of that first. According to The National Institute of Diabetes and Digestive and Kidney Diseases at
A GFR of 55 is the higher part of stage 3A. 60 is where stage 2 of CKD begins. My kidneys were functioning better on chemo. And the creatinine? Let’s get a quick definition of that first. According to The National Institute of Diabetes and Digestive and Kidney Diseases at 
 Oh, sorry, I didn’t give you the definition. This is from Healthline at
Oh, sorry, I didn’t give you the definition. This is from Healthline at 
 Her question? It’s about fiber and Chronic Kidney Disease. But first, let’s find out exactly what fiber is. According to Harvard’s T. H. Chan School of Public Health at
Her question? It’s about fiber and Chronic Kidney Disease. But first, let’s find out exactly what fiber is. According to Harvard’s T. H. Chan School of Public Health at
 ingredients and found this:
ingredients and found this:
 suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference.
suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference.
 AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”
AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”

 Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at
Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at 
 American Kidney Fund
American Kidney Fund  That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible.
That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible. Let’s see if I can find something more recent. This, from the National Kidney Fund at
Let’s see if I can find something more recent. This, from the National Kidney Fund at 
 When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
 Better Information
Better Information

 “Then I found this in BrightHub.com’s February 13th article The Importance of the Potassium and Sodium Balance.
“Then I found this in BrightHub.com’s February 13th article The Importance of the Potassium and Sodium Balance.
 Will she need extra medicines when she’s pregnant? Women trying to get pregnant should start taking the vitamin folic acid to reduce the chance of their baby having spina bifida, an abnormality of the spinal cord. The normal dose of folic acid is 400ug per day and can be bought over the counter. However, if the folate level is low or a patient is on the drug azathioprine which affects the way folic acid works, the dose of 5mg daily may be prescribed. No other over the counter vitamins are required unless specifically advised by a doctor or midwife. All pregnant patients should avoid additional supplements of vitamin A. If vitamin D levels are low GPs will advise correction with high dose prescribed vitamin D (also known as cholecalciferol). Women with kidney diseases are at higher risk of pre-eclampsia. Aspirin lowers the risk of pre eclampsia, and women with CKD are usually offered a low dose aspirin (75mg once daily) throughout pregnancy unless there are specific reasons not to take it e.g. they are allergic to aspirin. Pregnant women with a high level of protein in their urine have an increased risk of developing blood clots (thrombosis). This can be reduced by small daily injections of low molecular weight heparin. Heparin reduces the way the blood clots. Both pregnancy and CKD can cause a low blood count (
Will she need extra medicines when she’s pregnant? Women trying to get pregnant should start taking the vitamin folic acid to reduce the chance of their baby having spina bifida, an abnormality of the spinal cord. The normal dose of folic acid is 400ug per day and can be bought over the counter. However, if the folate level is low or a patient is on the drug azathioprine which affects the way folic acid works, the dose of 5mg daily may be prescribed. No other over the counter vitamins are required unless specifically advised by a doctor or midwife. All pregnant patients should avoid additional supplements of vitamin A. If vitamin D levels are low GPs will advise correction with high dose prescribed vitamin D (also known as cholecalciferol). Women with kidney diseases are at higher risk of pre-eclampsia. Aspirin lowers the risk of pre eclampsia, and women with CKD are usually offered a low dose aspirin (75mg once daily) throughout pregnancy unless there are specific reasons not to take it e.g. they are allergic to aspirin. Pregnant women with a high level of protein in their urine have an increased risk of developing blood clots (thrombosis). This can be reduced by small daily injections of low molecular weight heparin. Heparin reduces the way the blood clots. Both pregnancy and CKD can cause a low blood count ( Last weekend I was in Las Vegas renewing my vows to Bear as my brother and sister-in-law renewed their vows to each other. It was their 50th year of marriage, our 5th. I listened to what they had to say to each other during the ceremony and realized that was what I would have said to Bear on our 50th, if we were young enough to be able to count on having a 50th. And then I began to wonder how many people do reach this milestone in their lives.
Last weekend I was in Las Vegas renewing my vows to Bear as my brother and sister-in-law renewed their vows to each other. It was their 50th year of marriage, our 5th. I listened to what they had to say to each other during the ceremony and realized that was what I would have said to Bear on our 50th, if we were young enough to be able to count on having a 50th. And then I began to wonder how many people do reach this milestone in their lives.
 Lower estimated glomerular filtration rates???? No, thank you. I rarely go to casinos or any other place that allows smoking for that matter. I just don’t like the odor. Now I have a much more important reason to avoid such places.
Lower estimated glomerular filtration rates???? No, thank you. I rarely go to casinos or any other place that allows smoking for that matter. I just don’t like the odor. Now I have a much more important reason to avoid such places.
 This is from
This is from 
 It looks like I was wrong. Most of these are still available. Unfortunately KidneyDiet, my all-time favorite, is no more. Neither is Restaurant Nutrition. But let’s see what other apps are available for us.
It looks like I was wrong. Most of these are still available. Unfortunately KidneyDiet, my all-time favorite, is no more. Neither is Restaurant Nutrition. But let’s see what other apps are available for us. request reminders about your goal, as well as add foods. Of course, Premium offers you a lot more… and charges you accordingly. Articles about exercise and weight pop up, too. And then there are recipes. Again, it doesn’t do the whole trick, although it does count potassium, protein, sodium and calories . What’s missing is phosphorous. The bonuses are carb, fat (by type, no less) cholesterol, fiber, sugar, vitamins A & C, calcium, and iron counters. This is also a free Apple app.
request reminders about your goal, as well as add foods. Of course, Premium offers you a lot more… and charges you accordingly. Articles about exercise and weight pop up, too. And then there are recipes. Again, it doesn’t do the whole trick, although it does count potassium, protein, sodium and calories . What’s missing is phosphorous. The bonuses are carb, fat (by type, no less) cholesterol, fiber, sugar, vitamins A & C, calcium, and iron counters. This is also a free Apple app. Before I go, here’s a shameless plug for my new book. It’s
Before I go, here’s a shameless plug for my new book. It’s 
 I understood I had to limit my phosphorous, potassium, protein, and sodium to preserve my kidney function and was scared enough by my diagnosis to follow this diet religiously, recording the amounts I ate in a little notebook. Nowadays, there are apps that will help you track these electrolytes. I listed a few in
I understood I had to limit my phosphorous, potassium, protein, and sodium to preserve my kidney function and was scared enough by my diagnosis to follow this diet religiously, recording the amounts I ate in a little notebook. Nowadays, there are apps that will help you track these electrolytes. I listed a few in 
 • High-gas foods. If you experience bloating or gas, you might avoid items such as carbonated and alcoholic beverages, caffeine, raw fruit, and certain vegetables, such as cabbage, broccoli and cauliflower.
• High-gas foods. If you experience bloating or gas, you might avoid items such as carbonated and alcoholic beverages, caffeine, raw fruit, and certain vegetables, such as cabbage, broccoli and cauliflower.
 Merry Christmas… and for tomorrow, Happy Kwaanza. Oh, all right, let’s throw in Happy Chanukah although that’s already passed this year. What all these celebrations – yes, and New Year’s Eve, too – have in common is food. And food has potassium and phosphorous in it. Those are two of the electrolytes that Chronic Kidney Disease patients have to curtail.
Merry Christmas… and for tomorrow, Happy Kwaanza. Oh, all right, let’s throw in Happy Chanukah although that’s already passed this year. What all these celebrations – yes, and New Year’s Eve, too – have in common is food. And food has potassium and phosphorous in it. Those are two of the electrolytes that Chronic Kidney Disease patients have to curtail.

 I was going to give you my take on researching when I stumbled across Dr. Alicia White’s piece on the United Kingdom’s National Health Services site at
I was going to give you my take on researching when I stumbled across Dr. Alicia White’s piece on the United Kingdom’s National Health Services site at 
 Also, it’s important that the control group is as similar to the treated/exposed group as possible. The best way to achieve this is to randomly assign some people to be in the treated/exposed group and some people to be in the control group. This is what happens in a randomised controlled trial (RCT) and is why RCTs are considered the “gold standard” for testing the effects of treatments and exposures. … Without either, retain some healthy scepticism.
Also, it’s important that the control group is as similar to the treated/exposed group as possible. The best way to achieve this is to randomly assign some people to be in the treated/exposed group and some people to be in the control group. This is what happens in a randomised controlled trial (RCT) and is why RCTs are considered the “gold standard” for testing the effects of treatments and exposures. … Without either, retain some healthy scepticism.
 service and something she wanted to do. I was excited. Then she simply stopped emailing and answering calls. That was a couple of years ago.
service and something she wanted to do. I was excited. Then she simply stopped emailing and answering calls. That was a couple of years ago. Clarence Ferguson, RTSM, CMTA, NT
Clarence Ferguson, RTSM, CMTA, NT

 Big news!
Big news!