Now that I’m getting older [oh, all right, old], I see loads of specialists for my comorbidities. One of them, my rheumatologist, has mentioned several times that eGFR is lower in the summer and higher in the winter. I wondered why, but she’d already gone on to discussing my arthritis by the time I formulated my question. It seems like now is a good time to answer that question. Want to explore it with me?

A few reminders first. According to Medical News Today:
“A rheumatologist is an internal medicine doctor who specializes in diagnosing and treating inflammatory conditions that affect the joints, tendons, ligaments, bones, and muscles.
Rheumatologists diagnose and treat musculoskeletal conditions, but they do not perform surgery.”
I started seeing her for osteoarthritis decades ago.
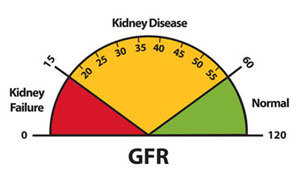
And eGFR? SelfCode, a site that is new to me which helps you decode your lab results, has that covered:
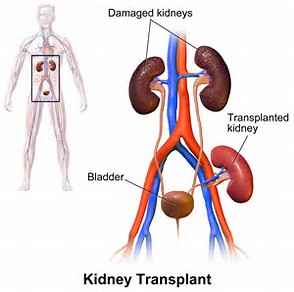
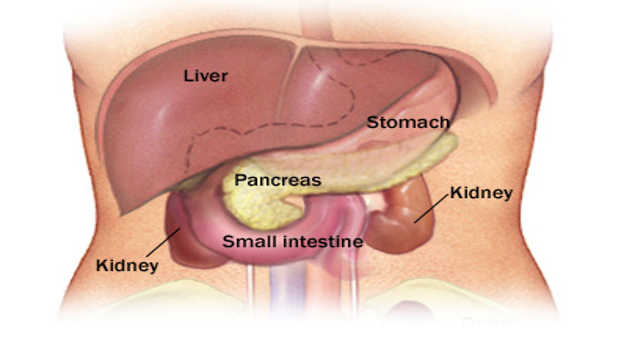
“Glomerular Filtration Rate (GFR) is the amount of blood filtered every minute by tiny filters in the kidneys called glomeruli. Although it may sound complicated, in essence, it measures how well your kidneys are working….”
Ready to explore the seasonal up and down of eGFR now? The first site that I could understand [Let’s remember I’m not a doctor and never claimed to be one.] which explained the connection between eGFR lowering during the summer was from the European Renal Association.

“In general, our body has various ways of regulating the body temperature and releasing excess heat. The best-known method is through sweating. If the temperature control centre in our brain, known as the ‘hypothalamus’, detects that our comfort body temperature of 37 degrees [That’s Celsius; it’s 98.6 Fahrenheit.] exceeded, the sweat glands in the skin are stimulated to produce more. We consequently give off heat by ‘evaporating’ the sweat on the surface of the body. In addition, the body dilates our skin vessels. The heart pumps more warm blood into the dilated skin vessels, which also dissipates heat.
The increased sweating naturally leads to a loss of fluid and important body salts, the so-called electrolytes. The lack of fluid and the heat-induced widening of the vessels lead to a drop in blood pressure. The heart no longer pumps enough blood through the body and the kidneys,” explains Professor Dr. Christoph Wanner, Head of Nephrology at the German University Hospital in Würzburg and President of the European Renal Association (ERA). ‘If you don’t compensate for this fluid loss, you become dehydrated. This can result in kidney failure. The risk to develop urinary stones and urinary tract infections is also bigger when the body is dehydrated.’”
Now this may look like it doesn’t address the question, but remember we need to keep hydrated to keep the eGFR up. Increased sweating is a factor. Losing fluid and electrolytes is a factor. Widening of the vessels is a factor. A drop in blood pressure is a factor. The kidneys not receiving enough blood is a factor.
Well, it seems my rheumatologist is right about lower eGFR in the summer. Wait a minute. That means she’s correct about a higher eGFR in the winter. Logically, if something is lower in some instances, it’s higher in others. Medically, we can work this backwards.
If the kidney disease patient is not abundantly sweating, then they are not losing fluid and electrolytes. If they are not losing fluid and electrolytes, their blood vessels are not widening. If their blood vessels are not widening, their blood pressure is not dropping. If their blood pressure is not dropping, the kidneys are receiving enough blood. If the kidneys are receiving enough blood, your eGFR will be higher than it would be if none of this were the case. Voila! There we have a higher [than summer] eGFR in the winter.
I thought it was interesting that blood pressure is also usually lower during the summer. The Mayo Clinic has the information on this:

“Blood pressure can be affected in summer weather because of the body’s attempts to radiate heat. High temperatures and high humidity can cause more blood flow to the skin. This causes the heart to beat faster while circulating twice as much blood per minute than on a normal day.
The greatest risks are when the temperature is above 70 degrees F and the humidity is more than 70%. The higher the humidity, the more moisture in the air.
Some people are at higher risk of being affected by humidity, including people over 50; those who are overweight; or those who have heart, lung or kidney conditions.
Heat and sweating also can lower the amount of fluid in the body, which can reduce blood volume and lead to dehydration. This can interfere with the body’s ability to cool off and may create strain on the heart.
Other risk factors include:
- Adults with heart, lung and kidney problems
- Seniors who follow a low-salt or low-sodium diet
- People who have a circulatory disease or problems with circulation
- Adults who take diuretics, sedatives and blood pressure medication”
Well now I understand why I thought I was going to pass out in Cuba. I live in Arizona, which has very low humidity. Cuba is high humidity. Lots of sweating going on at the time. Lots of drinking water, too, but apparently not enough.
We knew that high blood pressure could cause chronic kidney disease. Now we know that low blood pressure can affect your CKD.
Until next week,
Keep living your life!