That was my first thought when a reader asked me to write about nail fungus and chronic kidney disease. It was something I’d not only never thought about but had never occurred to me might be somehow connected to CKD.
Surprise! It is. Let’s start exploring it in our usual manner – with a definition. This is from the Mayo Clinic:
“Nail fungus is a common infection of the nail. It begins as a white or yellow-brown spot under the tip of your fingernail or toenail. As the fungal infection goes deeper, the nail may discolor, thicken and crumble at the edge. Nail fungus can affect several nails.”
This did not sound good at all. How, in heaven’s name, did this happen? WebMD had that topic thoroughly covered:
“You get an infection when a crack in your nail or the skin around it allows fungus to get inside and grow.
Since fungus thrives in dark, warm places, your toenails are more likely to be affected than your fingernails. Your toes also have less blood flow than your fingers, which makes it harder for your body to pick up on and prevent an infection.
You’re more likely to get a fungal nail infection if you:
- Are a man
- Are older, since nails become more brittle and likely to crack as you age
- Have a weak immune system or ongoing health problems like diabetes
- Wear shoes that make your feet hot and sweaty
- Walk barefoot through gym showers, swimming pools, and locker rooms –places where fungus spreads easily
- Live with someone who has a fungal infection
- Have athlete’s foot, as the fungus that causes it can spread to your nails
- Recently had an injury or surgery on your nail, or had a previous infection
- Wear plastic gloves or keep your hands wet for long periods”
As an older diabetic, I was getting a little bit more nervous the more I researched. I felt I needed to know the symptoms of nail fungus just as much as my reader did. So, I turned to Health.com only to find out there are different types of nail fungus with different symptoms:
“Any toenail fungus causes a range of symptoms, but some of the most common are: …
- Nail thickening
- Yellowing, browning, or discoloration
- Nail crumbling
- Abnormal or frequent breakage
- Unusually shaped nails
- Separation of the nail from the nail bed
- Pain
- Odor or bad smell

Different types of infections often cause various symptoms. For example, many mold infections aren’t painful, but yeast infections can be.
And you may notice a dark debris build-up under the nail with distal subungual toenail fungus. On the other hand, you’re more likely to see white spots or patches on the nail’s surface with white superficial toenail fungus….”
I also learned this was not something you could treat by yourself. According to the CDC:
“Fungal nail infections can be difficult to cure, and treatment is most successful when started early. Fungal nail infections typically don’t go away on their own, and the best treatment is usually prescription antifungal pills taken by mouth. In severe cases, a healthcare professional might remove the nail completely. It can take several months to a year for the infection to go away.
Fungal nail infections can be closely associated with fungal skin infections. If a fungal infection is not treated, it can spread from one place to the other. Patients should discuss all skin concerns with their healthcare provider to ensure that all fungal infections are properly treated.
Even after treatment, fungal nail infections can come back. This is more common in people who have conditions like diabetes that make them more likely to get a fungal nail infection. If you suspect an infection has returned, contact your healthcare provider.”
I was way more than halfway through writing this blog when I realized I hadn’t touched upon CKD’s role in nail fungus. It was time to rectify that. Where better to find this information than the National Nail Fungus Organization:
“Abnormal changes in nails are expected on people who are suffering from chronic kidney disease as their normal diets have also changed. Unless the patients are able to manage or slow down the progress of their kidney disease, their nails are not likely to improve.
Unfortunately, having CKD also makes them susceptible to acquiring nail fungus infection, and the risk increases for older persons and diabetic patients. For people with chronic kidney disease, they have limited options of nail fungus treatment. As their kidneys cannot flush out the toxins and clear the medications off their body, they must obtain their doctors’ approval and prescription for oral fungicidal medications.
They have the option of using topical treatments, though. And depending on the products’ ingredients, topical medications can just be as effective as oral ones without the side effects.”
While this was not exactly what I had been looking for, I deemed it important information for us to know. I also discovered that CKD does have other effects on your nails. I wanted to know why. Reset Kidney Health explained:
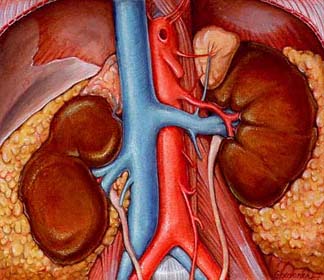
“The kidneys act as a filtration system, ridding our body of waste and delivering essential nutrients into our bloodstream. Unfortunately, as kidney disease progresses and function decreases, toxic substances will build up in our bloodstream and cause our nails to change color, form, and texture. High levels of nitrogen in the bloodstream often cause these physical changes.
Sometimes, chronic kidney disease sufferers will be placed on diets meant to slow the progression of the disease by limiting specific nutrient quantities to prevent a system overload on the already taxed kidneys. Unfortunately, that can result in nutrient deficiencies affecting keratin production, a protein responsible for nail strength.”
Makes sense to me. That could account for concave nails, yellow coloring, white streaking, Beau’s lines, detached, or brittle nails. I must admit I thoroughly enjoy learning about this particular side effect of CKD. I just don’t want to experience it, and I certainly hope you don’t either.
Until next week,
Keep living your life!


























 “Crystals in the urine is known as crystalluria. Sometimes crystals are found in healthy people and other times they are indicators of organ dysfunction, the presence of urinary tract stones of a like composition (known as urolithiasis), or an infection in the urinary tract.”
“Crystals in the urine is known as crystalluria. Sometimes crystals are found in healthy people and other times they are indicators of organ dysfunction, the presence of urinary tract stones of a like composition (known as urolithiasis), or an infection in the urinary tract.” makes sense that if the crystals do produce obstruction, the urine may back up… right into the kidneys. That’s when you have the AKI. Remember, this in not chronic. The condition remains until it’s remedied, but it can be remedied.
makes sense that if the crystals do produce obstruction, the urine may back up… right into the kidneys. That’s when you have the AKI. Remember, this in not chronic. The condition remains until it’s remedied, but it can be remedied. There is quite a bit more information about kidneys stones at this site. What we needed to know is that, again, it’s a buildup – as in not passed from the body via the urine – that causes kidney stones.
There is quite a bit more information about kidneys stones at this site. What we needed to know is that, again, it’s a buildup – as in not passed from the body via the urine – that causes kidney stones.

 “Constipation can be caused by a variety of medications. These medications affect the nerve and muscle activity in the large intestine (colon) and may also bind intestinal liquid. This may result in slowed colonic action (slow and/or difficult passing of stool).”
“Constipation can be caused by a variety of medications. These medications affect the nerve and muscle activity in the large intestine (colon) and may also bind intestinal liquid. This may result in slowed colonic action (slow and/or difficult passing of stool).”

 husband, who doesn’t have CKD, loved them, too. I enjoyed their pasta products, too. Now, lest you get the wrong idea, I am not endorsing this company because I don’t know what others like it are available. However, I wanted to know about their products… which may very well be similar to the products of other such companies and, therefore, helpful to CKD patients.
husband, who doesn’t have CKD, loved them, too. I enjoyed their pasta products, too. Now, lest you get the wrong idea, I am not endorsing this company because I don’t know what others like it are available. However, I wanted to know about their products… which may very well be similar to the products of other such companies and, therefore, helpful to CKD patients.
 from
from 

 *Glutathione is one of the body’s most important
*Glutathione is one of the body’s most important  Approximately 15% of all couples trying to conceive are affected by infertility. In almost half of these cases,
Approximately 15% of all couples trying to conceive are affected by infertility. In almost half of these cases, 
 “1. Avocado
“1. Avocado 
 This time I went to NDVTFoods at
This time I went to NDVTFoods at 
 “A chronic inflammatory disease that is caused by autoimmunity. Patients with
“A chronic inflammatory disease that is caused by autoimmunity. Patients with 
 Conservative treatments
Conservative treatments
 We all know diabetes raises your risk of developing Chronic Kidney Disease. But why? What’s the mechanism behind the fact? As far as I’m concerned, it’s time to find out.
We all know diabetes raises your risk of developing Chronic Kidney Disease. But why? What’s the mechanism behind the fact? As far as I’m concerned, it’s time to find out.
 good idea to limit red meat, and avoid processed meats.
good idea to limit red meat, and avoid processed meats.
 Let’s finish out this lazy, hazy summer month of August with another reader question. This one was quite straight forward:
Let’s finish out this lazy, hazy summer month of August with another reader question. This one was quite straight forward:

 “Healthy kidneys remove extra fluid and waste from your blood, but let proteins and other important nutrients pass through and return to your blood stream. When your kidneys are not working as well as they should, they can let some protein (albumin) escape through their filters, into your urine. When you have protein in your urine, it is called proteinuria (or albuminuria). Having protein in your urine can be a sign of nephrotic syndrome, or an early sign of kidney disease.”
“Healthy kidneys remove extra fluid and waste from your blood, but let proteins and other important nutrients pass through and return to your blood stream. When your kidneys are not working as well as they should, they can let some protein (albumin) escape through their filters, into your urine. When you have protein in your urine, it is called proteinuria (or albuminuria). Having protein in your urine can be a sign of nephrotic syndrome, or an early sign of kidney disease.”
 I was also given physical exercises to do, like raising my fisted hands above my head and straightening out my fist several times. This is one of many exercises. Do you remember the old TV show, E.R? It takes me slightly longer than one 43 minute episode to complete the exercises.
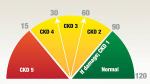
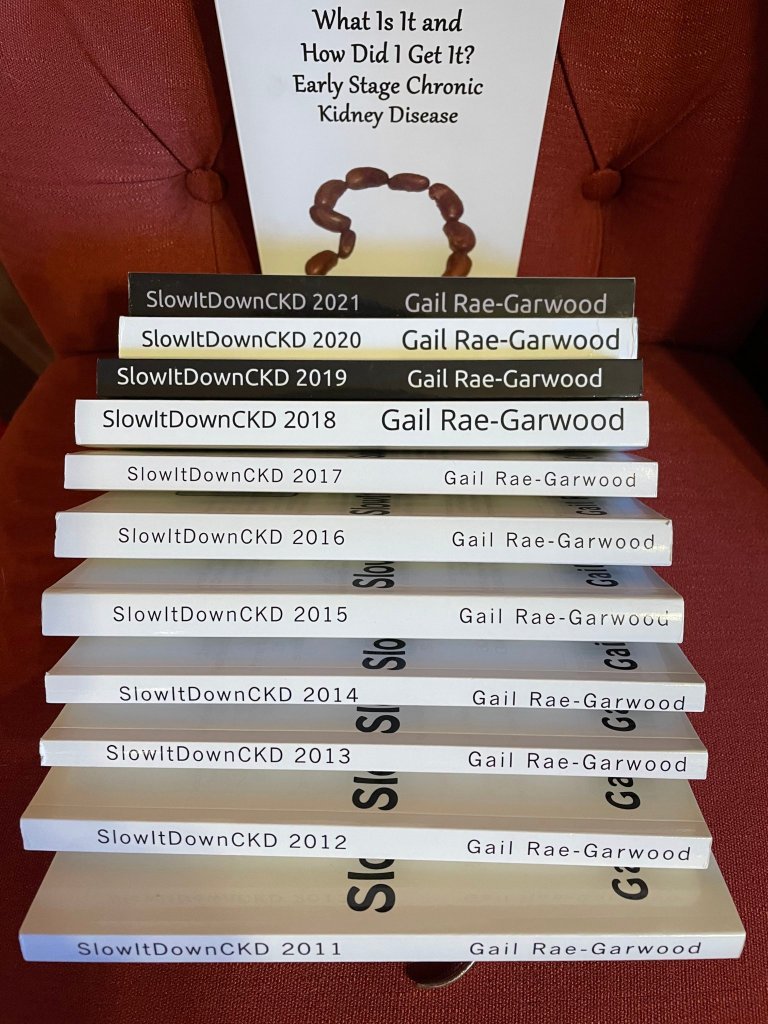
I was also given physical exercises to do, like raising my fisted hands above my head and straightening out my fist several times. This is one of many exercises. Do you remember the old TV show, E.R? It takes me slightly longer than one 43 minute episode to complete the exercises. As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book,
As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book, 
 A GFR of 55 is the higher part of stage 3A. 60 is where stage 2 of CKD begins. My kidneys were functioning better on chemo. And the creatinine? Let’s get a quick definition of that first. According to The National Institute of Diabetes and Digestive and Kidney Diseases at
A GFR of 55 is the higher part of stage 3A. 60 is where stage 2 of CKD begins. My kidneys were functioning better on chemo. And the creatinine? Let’s get a quick definition of that first. According to The National Institute of Diabetes and Digestive and Kidney Diseases at  National Kidney Month is just flying by. This is actually the last week and I doubt I’ll be able to post the rest of the 1in9 chapter before next month. But then again, it’s always Kidney Month for those of us with Chronic Kidney Disease. By the way, thank you to the reader who made it a point of telling me she can’t wait to read the rest of the chapter. Sooooo, let’s get started!
National Kidney Month is just flying by. This is actually the last week and I doubt I’ll be able to post the rest of the 1in9 chapter before next month. But then again, it’s always Kidney Month for those of us with Chronic Kidney Disease. By the way, thank you to the reader who made it a point of telling me she can’t wait to read the rest of the chapter. Sooooo, let’s get started!

 Exercise, something I loved until my arthritis got in the way, was also important. I was a dancer. Wasn’t that enough? Uh-uh, I had to learn about cardio and strength training exercise, too. It was no longer acceptable to be pleasantly plumb. My kidneys didn’t need the extra work. Hello to weights, walking, and a stationary bike. I think I took sleep for granted before CKD, too, and I now make it a point to get a good night’s sleep. A sleep apnea device improved my sleep—and my kidney function rose.
Exercise, something I loved until my arthritis got in the way, was also important. I was a dancer. Wasn’t that enough? Uh-uh, I had to learn about cardio and strength training exercise, too. It was no longer acceptable to be pleasantly plumb. My kidneys didn’t need the extra work. Hello to weights, walking, and a stationary bike. I think I took sleep for granted before CKD, too, and I now make it a point to get a good night’s sleep. A sleep apnea device improved my sleep—and my kidney function rose.
 That, of course, prompted me to go directly to the National Kidney Foundation’s information about National Kidney Month at
That, of course, prompted me to go directly to the National Kidney Foundation’s information about National Kidney Month at  I wanted to share this quote from the AKF with you, both as a CKD awareness advocate and a woman:
I wanted to share this quote from the AKF with you, both as a CKD awareness advocate and a woman: Oh, sorry, I didn’t give you the definition. This is from Healthline at
Oh, sorry, I didn’t give you the definition. This is from Healthline at 
 Tomorrow is Christmas and a Merry Christmas to those of you who celebrate. The day after Christmas Kwanzaa begins, so a Happy Kwanzaa to those of you who celebrate. But back to Christmas right now: today’s blog is a present to a reader who joined me way back when I first started blogging and has since become a close online friend.
Tomorrow is Christmas and a Merry Christmas to those of you who celebrate. The day after Christmas Kwanzaa begins, so a Happy Kwanzaa to those of you who celebrate. But back to Christmas right now: today’s blog is a present to a reader who joined me way back when I first started blogging and has since become a close online friend.
 “Kidney diseases or disorders can lead to high creatinine levels. Since the kidneys are the filters of wastes from the bloodstream, kidney damage means that there will be a buildup of creatinine beside other waste products in the body. Kidney conditions such as glomerulonephritis, acute tubular necrosis, kidney infection (pyelonephritis) and kidney failure can cause high creatinine levels. Reduced blood flow to the kidneys can also have a similar effect.
“Kidney diseases or disorders can lead to high creatinine levels. Since the kidneys are the filters of wastes from the bloodstream, kidney damage means that there will be a buildup of creatinine beside other waste products in the body. Kidney conditions such as glomerulonephritis, acute tubular necrosis, kidney infection (pyelonephritis) and kidney failure can cause high creatinine levels. Reduced blood flow to the kidneys can also have a similar effect. ask him not to, you say. Well, it’s involved. Basically, it’s because he has Alzheimer’s, doesn’t know how long winded he’s being, and feels terribly insulted when I ask him not to interrupt so I can write.
ask him not to, you say. Well, it’s involved. Basically, it’s because he has Alzheimer’s, doesn’t know how long winded he’s being, and feels terribly insulted when I ask him not to interrupt so I can write. energy. In Type 2 diabetes, either the pancreas does not make enough insulin or the body is unable to use insulin correctly.”
energy. In Type 2 diabetes, either the pancreas does not make enough insulin or the body is unable to use insulin correctly.” “Tau is one of two proteins—along with β-amyloid—that form unusual clumps in the brains of people with Alzheimer’s disease. Scientists have long debated which is most important to the condition and, thus, the best target for intervention. Tau deposits are found inside neurons, where they are thought to inhibit or kill them, whereas β-amyloid forms plaques outside brain cells.”
“Tau is one of two proteins—along with β-amyloid—that form unusual clumps in the brains of people with Alzheimer’s disease. Scientists have long debated which is most important to the condition and, thus, the best target for intervention. Tau deposits are found inside neurons, where they are thought to inhibit or kill them, whereas β-amyloid forms plaques outside brain cells.”


 suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference.
suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference.
 AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”
AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”

 pretty quickly, too. But then I noticed that I was hungry pretty much only after I ate.
pretty quickly, too. But then I noticed that I was hungry pretty much only after I ate.
 According the renal diet I follow, the Northern Arizona Council on Renal Nutrition Diet, I could eat all of these foods. According to my food sensitivities, I could only eat oatmeal, some fruits, and vegetables. Maybe that’s why eating makes me hungry.
According the renal diet I follow, the Northern Arizona Council on Renal Nutrition Diet, I could eat all of these foods. According to my food sensitivities, I could only eat oatmeal, some fruits, and vegetables. Maybe that’s why eating makes me hungry.
 When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
 Better Information
Better Information

 Oh, clone… as in Dolly, the sheep back in Scotland in 1995. Got it.
Oh, clone… as in Dolly, the sheep back in Scotland in 1995. Got it.




 I learned a new word! It’s gastroparesis. I learned it from the Facebook Chronic Kidney Disease support pages. What does it mean? According to the American Heritage Medical Dictionary, it means:
I learned a new word! It’s gastroparesis. I learned it from the Facebook Chronic Kidney Disease support pages. What does it mean? According to the American Heritage Medical Dictionary, it means:
 Last weekend I was in Las Vegas renewing my vows to Bear as my brother and sister-in-law renewed their vows to each other. It was their 50th year of marriage, our 5th. I listened to what they had to say to each other during the ceremony and realized that was what I would have said to Bear on our 50th, if we were young enough to be able to count on having a 50th. And then I began to wonder how many people do reach this milestone in their lives.
Last weekend I was in Las Vegas renewing my vows to Bear as my brother and sister-in-law renewed their vows to each other. It was their 50th year of marriage, our 5th. I listened to what they had to say to each other during the ceremony and realized that was what I would have said to Bear on our 50th, if we were young enough to be able to count on having a 50th. And then I began to wonder how many people do reach this milestone in their lives.
 Lower estimated glomerular filtration rates???? No, thank you. I rarely go to casinos or any other place that allows smoking for that matter. I just don’t like the odor. Now I have a much more important reason to avoid such places.
Lower estimated glomerular filtration rates???? No, thank you. I rarely go to casinos or any other place that allows smoking for that matter. I just don’t like the odor. Now I have a much more important reason to avoid such places.
 Have you heard of the Keto Diet? As a matter of fact, the app for that was included in last week’s blog. That’s one way to lose weight, but it’s too protein and fat heavy for CKD patients. Another way is to count carbohydrates or Bant.
Have you heard of the Keto Diet? As a matter of fact, the app for that was included in last week’s blog. That’s one way to lose weight, but it’s too protein and fat heavy for CKD patients. Another way is to count carbohydrates or Bant.

 Just in case you’re not sure which foods to avoid, Everyday Health at
Just in case you’re not sure which foods to avoid, Everyday Health at  This is from
This is from 
 It looks like I was wrong. Most of these are still available. Unfortunately KidneyDiet, my all-time favorite, is no more. Neither is Restaurant Nutrition. But let’s see what other apps are available for us.
It looks like I was wrong. Most of these are still available. Unfortunately KidneyDiet, my all-time favorite, is no more. Neither is Restaurant Nutrition. But let’s see what other apps are available for us. request reminders about your goal, as well as add foods. Of course, Premium offers you a lot more… and charges you accordingly. Articles about exercise and weight pop up, too. And then there are recipes. Again, it doesn’t do the whole trick, although it does count potassium, protein, sodium and calories . What’s missing is phosphorous. The bonuses are carb, fat (by type, no less) cholesterol, fiber, sugar, vitamins A & C, calcium, and iron counters. This is also a free Apple app.
request reminders about your goal, as well as add foods. Of course, Premium offers you a lot more… and charges you accordingly. Articles about exercise and weight pop up, too. And then there are recipes. Again, it doesn’t do the whole trick, although it does count potassium, protein, sodium and calories . What’s missing is phosphorous. The bonuses are carb, fat (by type, no less) cholesterol, fiber, sugar, vitamins A & C, calcium, and iron counters. This is also a free Apple app. Before I go, here’s a shameless plug for my new book. It’s
Before I go, here’s a shameless plug for my new book. It’s 
 I understood I had to limit my phosphorous, potassium, protein, and sodium to preserve my kidney function and was scared enough by my diagnosis to follow this diet religiously, recording the amounts I ate in a little notebook. Nowadays, there are apps that will help you track these electrolytes. I listed a few in
I understood I had to limit my phosphorous, potassium, protein, and sodium to preserve my kidney function and was scared enough by my diagnosis to follow this diet religiously, recording the amounts I ate in a little notebook. Nowadays, there are apps that will help you track these electrolytes. I listed a few in 


 Thursday is the American Thanksgiving. This is what we were taught in grade school when I was a child:
Thursday is the American Thanksgiving. This is what we were taught in grade school when I was a child: During holidays like Thanksgiving, people tend to eat very heavy meals with lots of proteins and carbohydrates, and this can impact not only kidney function, but also liver, pancreas and cardiac function,’ Mandayam said.
During holidays like Thanksgiving, people tend to eat very heavy meals with lots of proteins and carbohydrates, and this can impact not only kidney function, but also liver, pancreas and cardiac function,’ Mandayam said. Let’s talk about carbohydrates for a minute. I instantly think of bread, all kinds of bread which is even weirder because I’ve been on a low carb diet for a while. I know, you thought of cakes
Let’s talk about carbohydrates for a minute. I instantly think of bread, all kinds of bread which is even weirder because I’ve been on a low carb diet for a while. I know, you thought of cakes and pies, didn’t you? Did you know that fruits and vegetables contain carbohydrates, too?
and pies, didn’t you? Did you know that fruits and vegetables contain carbohydrates, too? Clarence Ferguson, RTSM, CMTA, NT
Clarence Ferguson, RTSM, CMTA, NT

 Big news!
Big news!