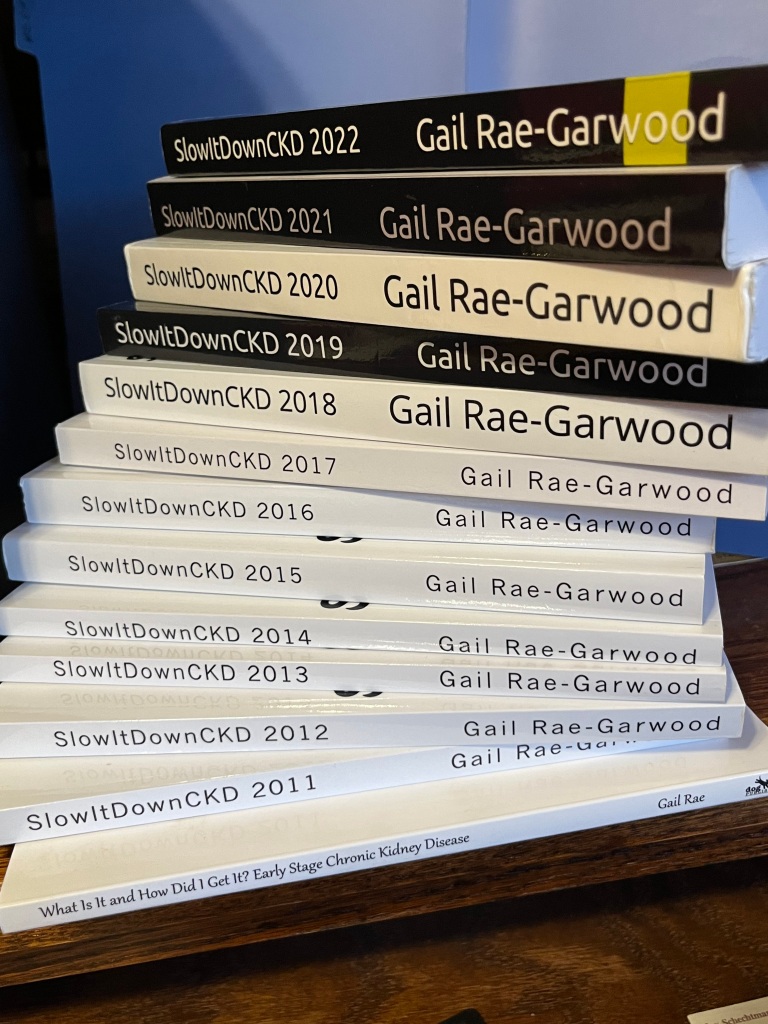
Last Thursday was World Kidney Day… and I’m late celebrating it. There are loads of medical issues in the family right now, but I’m trying to make up for this lapse. This past Saturday, I offered the digital versions of these books for free on Amazon:
What Is That and How Did I Get It? Early Stage Chronic Kidney
SlowItDownCKD 2011
SlowItDownCKD 2012
SlowItDownCKD 2013
SlowItDownCKD 2014
SlowItDownCKD 2015
SlowItDownCKD 2016
SlowItDownCKD 2018
SlowItDownCKD 2019
SlowItDownCKD 2020
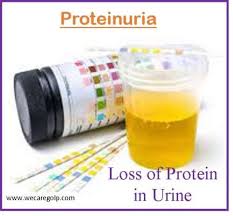
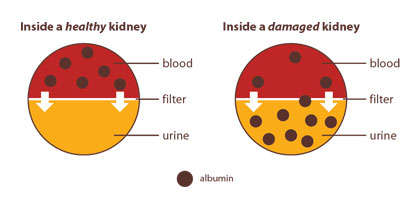
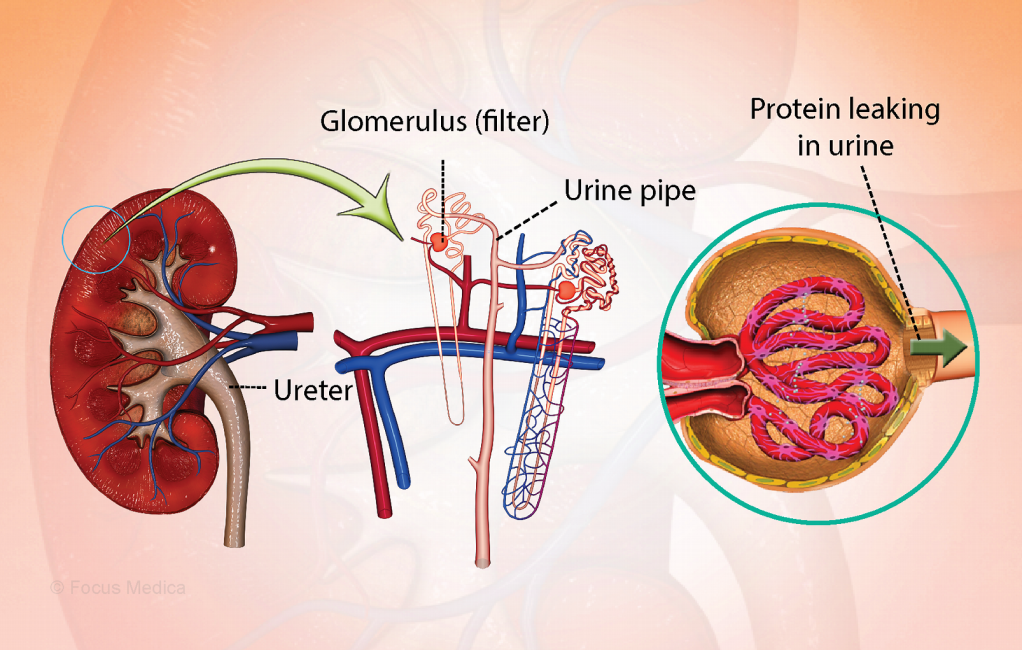
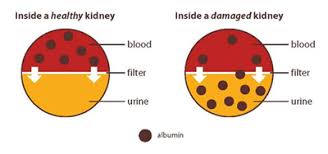
Why? Because 90% of people with chronic kidney disease don’t know they have it. I wanted them to know enough to realize that it’s worth a blood test and a urine test to be diagnosed. I also posted three reels publicizing this offer on social media. It’s that important to me that you find out for yourself whether or not you have CKD.
Then I thought we’d do something a little different this year and let World Kidney Day speak for itself:
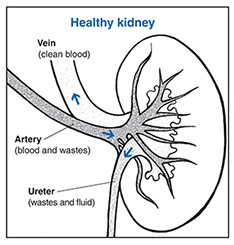
“World Kidney Day is a global campaign aimed at raising awareness of the importance of our kidneys.
World Kidney Day comes back every year. All across the globe many hundred events take place from public screenings in Argentina to Zumba marathons in Malaysia. We do it all to create awareness. Awareness about preventive behaviors, awareness about risk factors, and awareness about how to live with a kidney disease. We do this because we want kidney health for all.
World Kidney Day is a joint initiative of the International Society of Nephrology (ISN) and the International Federation of Kidney Foundations – World Kidney Alliance (IFKF-WKA)
…..
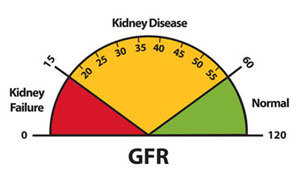
Advancing equitable access to care and optimal medication practice
Chronic kidney disease (CKD) is estimated to affect more than 850 million people worldwide and resulted in over 3.1 million deaths in 2019.[1] Presently, kidney disease ranks as the 8th leading cause of death[2], and if left unaddressed, it is projected to be the 5th leading cause of years of life lost by 2040.[3]
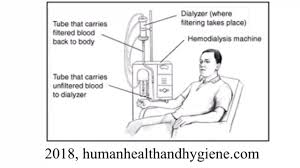
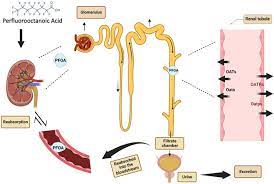
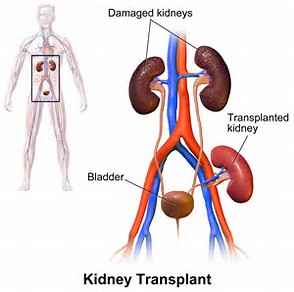
Over the last three decades, CKD treatment efforts have centered on preparing for and delivering kidney replacement therapies. However, recent therapeutic breakthroughs [4] offer unprecedented opportunities to prevent or delay disease and mitigate complications such as cardiovascular disease and kidney failure, ultimately prolonging the quality and quantity of life for people living with CKD.
While these new therapies should be universally accessible to all patients, in every country and environment, barriers such as lack of CKD awareness, insufficient knowledge or confidence with newer therapeutic strategies, shortages of kidney specialists, and treatment costs contribute to profound disparities in accessing treatments, particularly in low-and-middle-income countries, but also in some high-income settings. These inequities emphasize the need to shift focus towards CKD awareness and capacity building of the healthcare workforce.
Achieving optimal kidney care requires overcoming barriers at multiple levels while considering contextual differences across world regions. These include gaps in early diagnosis, lack of universal healthcare or insurance coverage, low awareness among healthcare workers, and challenges to medication cost and accessibility. A multi-pronged strategy is required to save kidneys, hearts, and lives:

- Health policies – Primary and secondary prevention of CKD require targeted health policies that holistically integrate kidney care into existing health programs, secure funding for kidney care, and disseminate kidney health knowledge to the public and the healthcare workforce. Equitable access to kidney disease screening, tools for early diagnosis, and sustainable access to quality treatment should be implemented to prevent CKD or its progression.
- Healthcare delivery – Suboptimal kidney care results from limited policy focus, inadequate patient and provider education, lack of resources for high-quality care, and limited access to affordable medication. To enact strategies successfully, it is essential to adopt a comprehensive, patient-centered, and locally oriented approaches to identify and remedy barriers to high-quality kidney care.
- Healthcare professionals – Addressing the shortage of primary care professionals and kidney specialists requires enhancing training, minimizing loss of healthcare providers, and building capacity among healthcare workers, including primary care physicians, nurses, and community health workers. Education on appropriate CKD screening and adherence to clinical practice guideline recommendations are key to successful implementation of effective and safe treatment strategies. Embracing scientific innovation and utilizing pharmacologic and non-pharmacologic tools for CKD treatment, as well as fostering effective communication and empathy among professionals would greatly impact patient well-being.
- Empowering patients and communities – Globally, patients struggle to access care and medication due to high costs and misinformation, which impact their health behaviors and adherence. Raising awareness about CKD risk factors such as diabetes, hypertension, and obesity, enhancing health literacy about healthy lifestyle choices, self-care, and promoting long-term adherence to treatment strategies can bring large benefits especially when initiated early and consistently maintained. Involving patients in advocacy organizations and local communities will empower them to make informed decisions and improve their health outcomes.
[1] https://vizhub.healthdata.org/gbd-results/
[2] https://www.healthdata.org/news-events/newsroom/news-releases/lancet-latest-global-disease-estimates-reveal-perfect-storm
[3] https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(18)31694-5.pdf
[4] Renin-angiotensin inhibitors, SGLT2 inhibitors, non-steroidal mineralocorticoid receptor antagonists, and GLP-1 receptor agonists, have shown benefits in delaying kidney function decline together with reducing risks of cardiovascular events and death.”
Re-reading this, I’m wondering if there’s a method to offer all the titles offered for free this past Saturday permanently free. That just might be a teeny bit of help in raising awareness about CKD risk factors.
Remember the kidney awareness work I do is my way of giving back for all the good in my life. What good? There’s surviving pancreatic cancer, meeting Bear, maintaining a close relationship with my children, having two grandsons, awaiting a new hip, keeping my CKD and diabetes under control, and – well – I could go on and on. Sure, there was bad in my life, too, but why waste energy dwelling on that?
Talking about good, here’s hoping you had a good, fun Saint Patrick’s Day. My children and grandsons called me to wish me a Happy Saint Patrick’s Day which automatically made it a Happy Saint Patrick’s Day.
World Kidney Day may have passed, but it’s still National Kidney Month here in the United States. Honoring that, in addition to the blog and books, I’ve agreed to a podcast interview in April and to attend a pharmaceutical conference in May.
Until next week,
Keep living your life!