Before we do anything else, Happy Birthday Nima (My New York Daughter). Okay, now we can start. Last week, we read the first part of Jim Myers’ guest blog about hearing loss and the kidneys. I promised then that we would finish his guest blog next week. This is next week, so take it away, Uncle Jim.

Hearing Loss and Meniere’s Disease
A Balance Assessment will take place.
Between vertigo attacks, balance returns to normal for most people with Meniere’s disease. But you might have some ongoing balance problems.
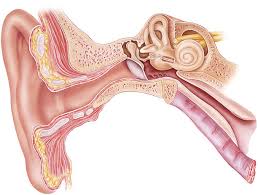
Tests that study how well the inner ear is working include:
Electronystagmogram or videonystagmography (ENG or VNG). These tests measure balance by studying eye movement. One part of the test looks at eye movement while your eyes follow a target. One part studies eye movement while your head is put in different positions. A third test, called the caloric test, follows eye movement by using temperature changes to trigger a reaction from the inner ear. Your healthcare provider may use warm and cold air or water in the ear for the caloric test.
No cure exists for Meniere’s disease. Some treatments can help lessen how bad vertigo attacks are and how long they last. But there are no treatments for permanent hearing loss. Your healthcare provider may be able to suggest treatments that prevent your hearing loss from getting worse.
Treatment Methods include:
Medicines for vertigo

Your healthcare provider may prescribe medicines to take during a vertigo attack so that it’s less severe:
• Motion sickness medicines. Medicines such as meclizine (Antivert) or diazepam (Valium) may lessen the spinning feeling and help control nausea and vomiting.
• Anti-nausea medicines. Medicines such as promethazine might control nausea and vomiting during a vertigo attack.
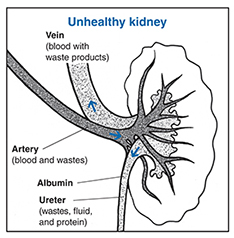
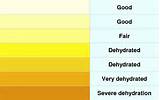
• Diuretics and betahistine. These medicines can be used together or alone to improve vertigo. Diuretics lower how much fluid is in the body, which may lower the amount of extra fluid in the inner ear. Betahistines ease vertigo symptoms by improving blood flow to the inner ear.
Long-term medicine use
Your healthcare provider may prescribe a medicine to reduce fluid retention and suggest limiting your salt intake. This helps control the intensity and amount of Meniere’s disease symptoms in some people.
Noninvasive therapies and procedures
Some people with Meniere’s disease may benefit from procedures that don’t include surgery, such as:
• Rehabilitation. If you have balance problems between vertigo attacks, vestibular rehabilitation therapy might improve your balance.
• Hearing aid. A hearing aid in the ear affected by Meniere’s disease might improve your hearing. Your healthcare provider can refer you to an ear doctor, also called an audiologist, to talk about the best hearing aids for you.
If conservative treatments aren’t successful, your care provider might suggest more-intense treatments.
Middle ear injections
Medicines injected and absorbed in the middle ear may help vertigo symptoms get better. This treatment is done in a care provider’s office. Injections can include:
• Gentamicin. This is an antibiotic that’s toxic to your inner ear. It works by damaging the sick part of your ear that’s causing vertigo. Your healthy ear then takes on the job for balance. But there is a risk of further hearing loss.
• Steroids. Steroids such as dexamethasone also may help control vertigo attacks in some people. Dexamethasone may not work as well as gentamicin. But it’s less likely to cause further hearing loss.
Surgery
If vertigo attacks from Meniere’s disease are severe and hard to bear and other treatments don’t help, surgery might be an option. Procedures include:
• Endolymphatic sac surgery. The endolymphatic sac helps control inner ear fluid levels. This procedure relieves pressure around the endolymphatic sac, which can improve fluid levels. Sometimes, a care provider places a tube inside your ear to drain any extra fluid.
• Labyrinthectomy. With this procedure, the surgeon removes the parts of your ear causing vertigo, which causes complete hearing loss in that ear. This allows your healthy ear to be in charge of sending information about balance and hearing to your brain. Care providers only suggest this procedure if you have poor hearing or total hearing loss in the diseased ear.
• Vestibular nerve section. This procedure involves cutting the vestibular nerve to prevent information about movement from getting to the brain. The vestibular nerve sends balance and movement information from your inner ear to the brain. This procedure usually improves vertigo and keeps hearing in the diseased ear. Most people need medicine that puts them in a sleep-like state, called general anesthesia, and an overnight hospital stay.
What illness causes hearing damage?
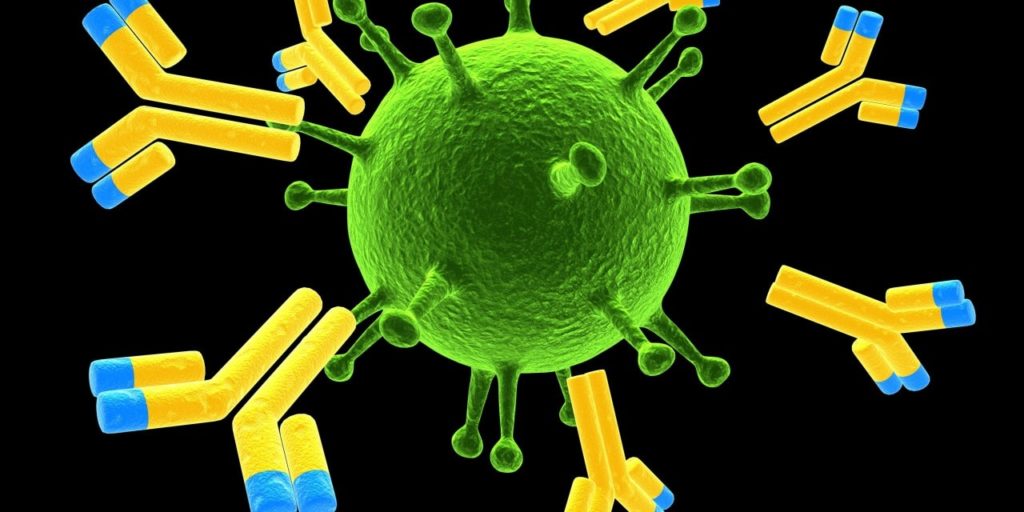
Certain diseases can cause hearing loss, including meningitis, mumps, cytomegalovirus and chickenpox. Severe cases of jaundice can also cause hearing loss. other causes – other causes of deafness include Meniere’s disease and exposure to certain chemicals.
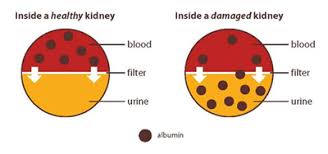
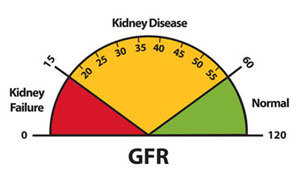
There is a significant relationship between CKD and Hearing Loss. One recent article states, “Patients with CKD are predisposed to several otorhinolaryngological issues especially SNHL, and the link between SNHL (sensorineural hearing loss)
and CKD has both been extensively explained, but the relationship between the remaining complications and CKD is still unknown.”
In plain English, if you suffer from CKD, you should get your hearing checked, and if you have any symptoms that we have discussed today, you may wish to consult with an otolaryngologist.
Several studies harmful effects of chronic kidney disease (CKD) on the audiovestibular system. This would include a connection between Chronic Kidney Disease and Meniere’s Disease. Patients with CKD had a significantly increased incidence of Ménière’s disease,
According to the Mayo Clinic, Meniere’s disease is an inner ear problem that can cause dizzy spells, also called vertigo, and hearing loss. Most of the time, Meniere’s disease affects only one ear.
Meniere’s disease can happen at any age. But it usually starts between the ages of 40 to 60. It’s thought to be a lifelong condition. But some treatments can help ease symptoms and lessen how it affects your life long term.
Symptoms of Meniere’s disease include:
• Regular dizzy spells. You have a spinning feeling that starts and stops suddenly. Vertigo may start without warning. It usually lasts 20 minutes to 12 hours, but not more than 24 hours. Serious vertigo can cause nausea.
• Hearing loss. Hearing loss in Meniere’s disease may come and go, especially early on. Over time, hearing loss can be long-lasting and not get better.
• Ringing in the ear. Ringing in the ear is called tinnitus. Tinnitus is the term for when you have a ringing, buzzing, roaring, whistling or hissing sound in your ear.
• Feeling of fullness in the ear. People with Meniere’s disease often feel pressure in the ear. This is called aural fullness.
After a vertigo attack, symptoms get better and might go away for a while. Over time, how many vertigo attacks you have may lessen.
To Diagnose Meniere’s, the physician will conduct an exam and asks about your health history. A Meniere’s disease diagnosis needs to include:
• Two or more vertigo attacks, each lasting 20 minutes to 12 hours, or up to 24 hours.
• Hearing loss proved by a hearing test.
• Tinnitus or a feeling of fullness or pressure in the ear.
Gail here: Jim has some really good resources if you’re interested. Let me know which area caught your interest.
Until next week,
Keep living your life!