When I first stumbled upon this word, I thought it might have something to do with marriage since the initial syllable of husband is hus. According to Vocabulary.com,
“The word husband comes from the Old Norse hūsbōndi, where hūs meant house and bōndi meant dweller.”
But then, I looked up aHus. Was I ever wrong in assuming this had to do with a house. I turned to my trusted favorites to see what I could find out about this word I hadn’t heard before, starting with the American Kidney Fund:
“aHUS (atypical hemolytic uremic syndrome) is a very rare disease that causes tiny blood clots to form in the small blood vessels of your body. These blood clots can block blood flow to important organs, such as your kidneys. This can damage your kidneys and lead to kidney failure.”
I’m pretty sure we all know what atypical and syndrome mean. Just in case you forgot, uremic means of or about the urine. And hemolytic? That means blood (hemo) and lysis (rupturing). Or in this case, “rupturing of the red blood cells and the release of their contents into the surrounding fluid.” Thanks for helping us out here, Wikipedia. While this was the most reader friendly definition I could find, keep in mind that anyone can edit a Wikipedia entry.
So, we’re back in the realm of rare diseases. I’d like to know what causes this particular rare disease. Since it is a rare disease, I went to GARD’s website for information about how one gets this disease. By the way, GARD is the new website for Genetic and Rare Diseases and is part of National Center for Advancing Translational Sciences. That’s part of the U.S. Department of Health and Human Services’ National Institutes of Health.
“It can occur at any age and is often caused by a combination of environmental and genetic factors. Genetic factors involve genes that code for proteins that help control the complement system (part of your body’s immune system). Environmental factors include certain medications (such as anticancer drugs), chronic diseases (e.g., systemic sclerosis and malignant hypertension), viral or bacterial infections, cancers, organ transplantation, and pregnancy. In about 60% of aHUS, a genetic change may be identified. The genes associated with genetic aHUS include C3, CD46 (MCP), CFB, CFH, CFHR1, CFHR3, CFHR4, CFI, DGKE, and THBD. Genetic changes in these genes increase the likelihood (predisposition) to developing aHUS, rather than directly causing the disease. In most cases, there is no family history of the disease. In cases that do run in families, predisposition to aHUS is inherited in an autosomal dominant or an autosomal recessive pattern of inheritance.”
Uh-oh, did you notice ‘organ transplantation’ as one of the environmental factors which may cause this disease? And ‘chronic disease’? That makes it even more important for us to know how to recognize if we have this disease. Well, how do we do that?
I went to the site called aHusNews to see if they could pinpoint the symptoms. Sure enough, they could.
“Often, people with aHUS will report a vague feeling of illness, with non-specific symptoms that may include paleness, nausea, vomiting, fatigue, drowsiness, high blood pressure, and swelling.
There are three hallmark symptoms that define aHUS: hemolytic anemia, thrombocytopenia, and kidney failure.
Symptoms can appear at any age, though it is slightly more common for them to first appear in childhood rather than later on in life. Adult-onset aHUS is more frequent in biological females than males, whereas childhood-onset disease affects both sexes equally.”
Is that how it’s diagnosed, I wondered. A different site, called Ahus.org was helpful here.
“…. After initial blood tests, the hospital may conduct Creatinine and BUN tests and may (or may not) reach an initial Diagnosis of atypical HUS. The flu like symptoms … will continue to worsen when episodes are active. At this point, kidney function may begin to fall, often quite dramatically. Other organs sometime experience problems in some cases. Quite often, seizures have been reported, along with other neurological issues. Sometimes gastronomical problems occur as well.
During an extended atypical attack or episode, the tell-tale signs of aHUS are very obvious. Hemoglobin levels may fall to 6-7, when normal levels should be 11-13: Hematocrit levels may fall in the low 20s, when normal levels should be in the mid 30s. Creatinine and BUN levels start to rise, characteristics of failing kidney function. Blood Pressure will become a nagging, recurring problem. Diarrhea and vomiting may also be present (sometimes that occurs with the initial onset, at other times it occurs later) ….
TRIGGERS VS. THE CAUSE
It is important not to confuse ‘triggers’ of atypical HUS with the root cause. In normal life, many of us get colds, the flu, infections, and the body’s immune system deal with those properly. In aHUS, a person may get a cold, and it triggers a full blown aHUS episode. This occurs simply because the body’s immune system is not reacting properly to the event.”
The site mentions other specific tests that may be done to diagnose aHus.
All this is worrisome. Is there, perhaps, a cure? No, there isn’t. This is a lifelong disease, but there are treatments available. Our old friend WebMD explains:
” The FDA has approved two drugs to treat aHUS:
Eculizumab (Soliris)
Ravulizumab (Ultomirus)
Both drugs are monoclonal antibodies. These are human-made proteins that act like natural antibody proteins in your body. They attach to other proteins called antigens. Once they attach, they tell your immune system to destroy cells with that antigen.
Eculizumab can increase your blood platelet and red blood cell counts. If you take it early enough, it can also reverse any kidney damage you have.
Your doctor will give you eculizumab by injection in their office. You may have side effects from the drug…. You can also get ravulizumab as an injection. Common side effects include high blood pressure, headache, and cold symptoms. You could also have digestive system problems such as diarrhea, nausea, and vomiting.
Eculizumab and ravulizumab are a type of drug called complement inhibitors. These kinds of drugs may carry a risk of getting meningococcal disease. The CDC suggests people taking them get a meningococcal vaccine. Your doctor may also suggest you take antibiotics to help prevent meningococcal disease.
Besides eculizumab and ravulizumab, you can also treat the symptoms of aHUS with plasma therapy. Plasma is a liquid portion of your blood that takes important nutrients, hormones, and proteins throughout your body.
When you get plasma therapy, you may either have a plasma infusion or plasma exchange.
In a plasma infusion, a doctor puts plasma from a donor into your body. In a plasma exchange, a doctor filters plasma parts out of your blood and replaces them with donor plasma.
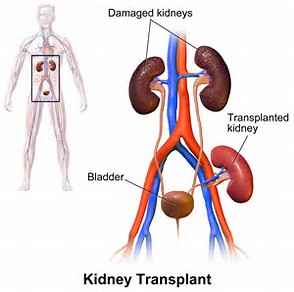
If your kidneys don’t respond to treatment, you may need kidney dialysis or a kidney transplant.”
Now you know, whether you wanted to or not. I’m sorry.
Until next week,
Keep living your life!




































 his army across the
his army across the  A computerized tomography (CT) scan combines a series of X-ray images taken from different angles around your body and uses computer processing to create cross-sectional images (slices) of the bones, blood vessels and soft tissues inside your body. CT scan images provide more-detailed information than plain X-rays do.”
A computerized tomography (CT) scan combines a series of X-ray images taken from different angles around your body and uses computer processing to create cross-sectional images (slices) of the bones, blood vessels and soft tissues inside your body. CT scan images provide more-detailed information than plain X-rays do.” Of course, now we need to know why we shouldn’t be having this contrast material. Radiology Affiliates Imagining at
Of course, now we need to know why we shouldn’t be having this contrast material. Radiology Affiliates Imagining at 

 It seems that most of them are taking lithium to help control the bipolar disorder. Okay, I’ll bite: what is lithium? Drugs.com at
It seems that most of them are taking lithium to help control the bipolar disorder. Okay, I’ll bite: what is lithium? Drugs.com at 
 The most common problem from taking lithium is a form of diabetes due to kidney damage called nephrogenic diabetes insipidus. This type of diabetes is different than diabetes mellitus caused by high blood sugar. In nephrogenic diabetes insipidus, the kidneys cannot respond to anti-diuretic hormone (ADH), a chemical messenger that controls fluid balance. This results in greater than normal urine out-put and excessive thirst. It can be hard to treat nephrogenic diabetes insipidus.”
The most common problem from taking lithium is a form of diabetes due to kidney damage called nephrogenic diabetes insipidus. This type of diabetes is different than diabetes mellitus caused by high blood sugar. In nephrogenic diabetes insipidus, the kidneys cannot respond to anti-diuretic hormone (ADH), a chemical messenger that controls fluid balance. This results in greater than normal urine out-put and excessive thirst. It can be hard to treat nephrogenic diabetes insipidus.”
 On October 1st, 2018, I explored the menstrual cycle’s effect on CKD and vice-versa issue:
On October 1st, 2018, I explored the menstrual cycle’s effect on CKD and vice-versa issue: ‘Women with CKD have been shown to commonly experience menstrual irregularities. This can include excessive bleeding, missed periods, and early onset of menopause. In studies of patients with CKD, women enter menopause from 3 to 5 years earlier than patients without CKD. Treatment can be very challenging. Studies of estrogen replacement therapy have shown an increased risk of heart disease and blood clotting disorders. Kidney transplantation will usually correct these abnormalities.’
‘Women with CKD have been shown to commonly experience menstrual irregularities. This can include excessive bleeding, missed periods, and early onset of menopause. In studies of patients with CKD, women enter menopause from 3 to 5 years earlier than patients without CKD. Treatment can be very challenging. Studies of estrogen replacement therapy have shown an increased risk of heart disease and blood clotting disorders. Kidney transplantation will usually correct these abnormalities.’




 That’s a pretty big build up for a common sense question. But, at least now you understand how I handle reader questions and may want to ask one (or more) of your own.
That’s a pretty big build up for a common sense question. But, at least now you understand how I handle reader questions and may want to ask one (or more) of your own.

 Let’s start at the beginning. FSGS is the acronym for focal segmental glomerulosclerosis. Anything look familiar? Maybe the ‘glomerul’ part of glomerulosclerosis? I think we need to know the definition of glomerulosclerosis to be able to answer that question. The National Institutes of Health’s U.S. National Library of Congress’s Medline Plus at
Let’s start at the beginning. FSGS is the acronym for focal segmental glomerulosclerosis. Anything look familiar? Maybe the ‘glomerul’ part of glomerulosclerosis? I think we need to know the definition of glomerulosclerosis to be able to answer that question. The National Institutes of Health’s U.S. National Library of Congress’s Medline Plus at 

 I think we need another definition here. Yep, it’s Plasmapheresis. Back to the Encarta Dictionary.
I think we need another definition here. Yep, it’s Plasmapheresis. Back to the Encarta Dictionary. As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book,
As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book, 
 National Kidney Month is just flying by. This is actually the last week and I doubt I’ll be able to post the rest of the 1in9 chapter before next month. But then again, it’s always Kidney Month for those of us with Chronic Kidney Disease. By the way, thank you to the reader who made it a point of telling me she can’t wait to read the rest of the chapter. Sooooo, let’s get started!
National Kidney Month is just flying by. This is actually the last week and I doubt I’ll be able to post the rest of the 1in9 chapter before next month. But then again, it’s always Kidney Month for those of us with Chronic Kidney Disease. By the way, thank you to the reader who made it a point of telling me she can’t wait to read the rest of the chapter. Sooooo, let’s get started!

 Exercise, something I loved until my arthritis got in the way, was also important. I was a dancer. Wasn’t that enough? Uh-uh, I had to learn about cardio and strength training exercise, too. It was no longer acceptable to be pleasantly plumb. My kidneys didn’t need the extra work. Hello to weights, walking, and a stationary bike. I think I took sleep for granted before CKD, too, and I now make it a point to get a good night’s sleep. A sleep apnea device improved my sleep—and my kidney function rose.
Exercise, something I loved until my arthritis got in the way, was also important. I was a dancer. Wasn’t that enough? Uh-uh, I had to learn about cardio and strength training exercise, too. It was no longer acceptable to be pleasantly plumb. My kidneys didn’t need the extra work. Hello to weights, walking, and a stationary bike. I think I took sleep for granted before CKD, too, and I now make it a point to get a good night’s sleep. A sleep apnea device improved my sleep—and my kidney function rose. Tomorrow is Christmas and a Merry Christmas to those of you who celebrate. The day after Christmas Kwanzaa begins, so a Happy Kwanzaa to those of you who celebrate. But back to Christmas right now: today’s blog is a present to a reader who joined me way back when I first started blogging and has since become a close online friend.
Tomorrow is Christmas and a Merry Christmas to those of you who celebrate. The day after Christmas Kwanzaa begins, so a Happy Kwanzaa to those of you who celebrate. But back to Christmas right now: today’s blog is a present to a reader who joined me way back when I first started blogging and has since become a close online friend.
 “Kidney diseases or disorders can lead to high creatinine levels. Since the kidneys are the filters of wastes from the bloodstream, kidney damage means that there will be a buildup of creatinine beside other waste products in the body. Kidney conditions such as glomerulonephritis, acute tubular necrosis, kidney infection (pyelonephritis) and kidney failure can cause high creatinine levels. Reduced blood flow to the kidneys can also have a similar effect.
“Kidney diseases or disorders can lead to high creatinine levels. Since the kidneys are the filters of wastes from the bloodstream, kidney damage means that there will be a buildup of creatinine beside other waste products in the body. Kidney conditions such as glomerulonephritis, acute tubular necrosis, kidney infection (pyelonephritis) and kidney failure can cause high creatinine levels. Reduced blood flow to the kidneys can also have a similar effect. By now it shouldn’t surprise me that as I’m out and about I’m constantly meeting more and more people with a connection to kidney disease. That was not the case 21 years ago, or even four years ago for that matter. What changed? The opening of my eyes to statistics I was previously unaware of, and frankly I found to be quite shocking and unacceptable. I’ll get to those stats a little later.
By now it shouldn’t surprise me that as I’m out and about I’m constantly meeting more and more people with a connection to kidney disease. That was not the case 21 years ago, or even four years ago for that matter. What changed? The opening of my eyes to statistics I was previously unaware of, and frankly I found to be quite shocking and unacceptable. I’ll get to those stats a little later.
 kidneys failed! He and his dance partner and instructor, Brianna Santiago, spent six months of grueling practices preparing for their energetic performance to Pharrell William’s song Happy, demonstrating the improved quality of life home dialysis can provide, and that dialysis does not have to be a death sentence.
kidneys failed! He and his dance partner and instructor, Brianna Santiago, spent six months of grueling practices preparing for their energetic performance to Pharrell William’s song Happy, demonstrating the improved quality of life home dialysis can provide, and that dialysis does not have to be a death sentence. University of Arizona
University of Arizona  You’d think that leaves me out, but you’d be wrong. I’m writing for pre-menopausal women…and for anyone who wants to know what menstrual cycles have to do with Chronic Kidney Disease. I’m one of those who wants to know.
You’d think that leaves me out, but you’d be wrong. I’m writing for pre-menopausal women…and for anyone who wants to know what menstrual cycles have to do with Chronic Kidney Disease. I’m one of those who wants to know. Whoa! I wouldn’t want even more of these substances in my body. Not only would they make the CKD worse, but also its effects on my body. According to Medical News Today at
Whoa! I wouldn’t want even more of these substances in my body. Not only would they make the CKD worse, but also its effects on my body. According to Medical News Today at  okay, I guess that sort of makes sense. And then, oh my, I developed diabetes. But how? I’d never questioned how that worked before, but I certainly did now.
okay, I guess that sort of makes sense. And then, oh my, I developed diabetes. But how? I’d never questioned how that worked before, but I certainly did now.
 I would say I’m heart… uh, kidney…broken about this development, but the truth is I’m not. I don’t like it; I don’t want it, but I can do something about it. I’d already cut out complex carbs and sugar laden foods in an abortive attempt to lose weight for my health. Well, maybe my daughter’s wedding on October 6th had something to do with that decision, too.
I would say I’m heart… uh, kidney…broken about this development, but the truth is I’m not. I don’t like it; I don’t want it, but I can do something about it. I’d already cut out complex carbs and sugar laden foods in an abortive attempt to lose weight for my health. Well, maybe my daughter’s wedding on October 6th had something to do with that decision, too. suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference.
suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference.
 AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”
AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”

 Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at
Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at 
 American Kidney Fund
American Kidney Fund  That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible.
That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible. Let’s see if I can find something more recent. This, from the National Kidney Fund at
Let’s see if I can find something more recent. This, from the National Kidney Fund at 
 When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
 Better Information
Better Information
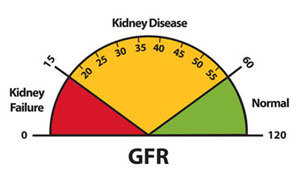
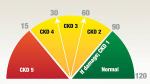 decline in our kidney function. I maintain that if only my primary care physician had told me when he first noticed that 39% GFR, maybe I wouldn’t be in stage 3 of 5. Maybe those now on dialysis or searching for a transplant wouldn’t be in the position they are, either.
decline in our kidney function. I maintain that if only my primary care physician had told me when he first noticed that 39% GFR, maybe I wouldn’t be in stage 3 of 5. Maybe those now on dialysis or searching for a transplant wouldn’t be in the position they are, either.
 The literature suggests early nephrologist involvement improves long-term outcomes. Proactive primary care offers longitudinal guidance for making the enormous lifestyle changes in diet, exercise, stress management, hydration, sleep and toxic exposures, while offering psychological counseling that is required to achieve such changes. The cross-over benefits for patients’ other diagnoses is well known.
The literature suggests early nephrologist involvement improves long-term outcomes. Proactive primary care offers longitudinal guidance for making the enormous lifestyle changes in diet, exercise, stress management, hydration, sleep and toxic exposures, while offering psychological counseling that is required to achieve such changes. The cross-over benefits for patients’ other diagnoses is well known.

 How Does It Work?
How Does It Work?
 We do need to start with some basics here. First, what is chemotherapy? According to the American Cancer Society at
We do need to start with some basics here. First, what is chemotherapy? According to the American Cancer Society at 

 This does address older adults which is why I believe they mention age as a CKD risk factor. We know that’s not the only risk factor.
This does address older adults which is why I believe they mention age as a CKD risk factor. We know that’s not the only risk factor.
























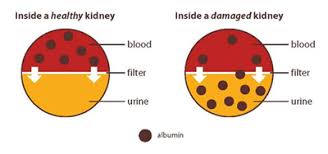
 A friend called me Friday night wondering what her creatinine/albumin ratio meant since that reading was high on her last blood draw. Actually, she wanted to know if this was something to worry about. After extracting a promise that she would call her doctor with her questions today when her physician’s office opened for business again, I gave her some explanations. Of course, then I wanted to give you the same explanations.
A friend called me Friday night wondering what her creatinine/albumin ratio meant since that reading was high on her last blood draw. Actually, she wanted to know if this was something to worry about. After extracting a promise that she would call her doctor with her questions today when her physician’s office opened for business again, I gave her some explanations. Of course, then I wanted to give you the same explanations.

 present a poster about it during the conference this past weekend. In addition I was lucky enough to have lunch with one of the keynote speakers. Who, you ask? Amy D. Waterman, Ph.D.
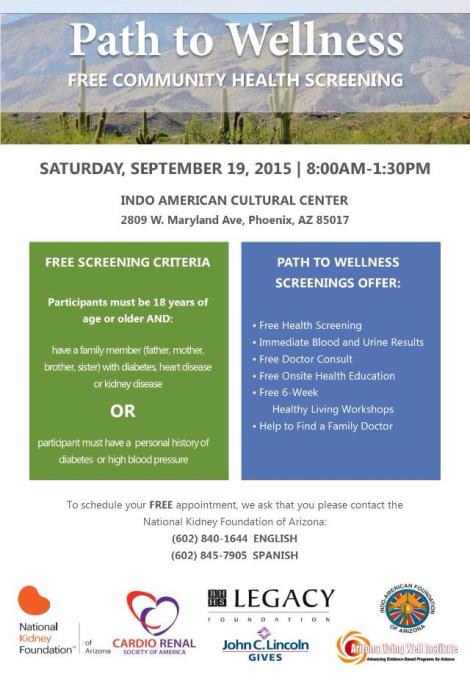
present a poster about it during the conference this past weekend. In addition I was lucky enough to have lunch with one of the keynote speakers. Who, you ask? Amy D. Waterman, Ph.D. Lest we forget, this year’s first Path of Wellness Screening will be Saturday, June 17th at the Indo American Cultural Center’s community hall, 2809 W. Maryland Ave., Phoenix, AZ 85017. As they’ve stated, “The free screening events can process up to 200 people. Their use of point-of-care testing devices provides blood and urine test results in a matter of minutes, which are reviewed onsite by volunteer physicians. All screening participants are offered free enrollment in chronic disease self-management workshops. Help is also given to connect participants with primary care resources. The goals of PTW are to improve early identification of at-risk people, facilitate their connection to health care resources, and slow the progression of chronic diseases in order to reduce heart failure, kidney failure and the need for dialysis.”
Lest we forget, this year’s first Path of Wellness Screening will be Saturday, June 17th at the Indo American Cultural Center’s community hall, 2809 W. Maryland Ave., Phoenix, AZ 85017. As they’ve stated, “The free screening events can process up to 200 people. Their use of point-of-care testing devices provides blood and urine test results in a matter of minutes, which are reviewed onsite by volunteer physicians. All screening participants are offered free enrollment in chronic disease self-management workshops. Help is also given to connect participants with primary care resources. The goals of PTW are to improve early identification of at-risk people, facilitate their connection to health care resources, and slow the progression of chronic diseases in order to reduce heart failure, kidney failure and the need for dialysis.”