Our old friend, Leesa Thompson …. Wait a minute! I don’t mean you’re old, Leesa. I mean we’ve had a couple of guest blogs from you before. Please forgive me. Anyway, Leesa has brought another guest blog to me. This one is perfect for National Kidney Month and a lovely way to end this celebratory month. Take it away, Leesa…
National Kidney Month is observed annually in March to raise awareness about kidney health, kidney disease prevention, and the importance of early detection and treatment. During this month-long observance, various organizations, including the National Kidney Foundation (NKF) and the American Kidney Fund (AKF), as well as healthcare providers and advocates, work to educate the public about kidney health and the risk factors associated with kidney disease. The primary goals of National Kidney Month are to:
1. Raise Awareness: National Kidney Month aims to increase awareness about the importance of kidney health and the prevalence of kidney disease, which affects millions of people worldwide. By educating the public about the risk factors, symptoms, and complications of kidney disease, advocates hope to encourage individuals to take proactive steps to protect their kidney health.
2. Promote Prevention: Kidney disease is often preventable or manageable when detected early. National Kidney Month provides an opportunity to promote healthy lifestyle habits, such as maintaining a balanced diet, staying hydrated, exercising regularly, managing blood pressure and blood sugar levels, and avoiding tobacco use, which can help reduce the risk of developing kidney disease.
3. Support Patients: National Kidney Month also serves as a platform to show support for individuals living with kidney disease and those who have undergone kidney transplantation. It highlights the importance of access to quality healthcare, treatment options, and support services for kidney disease patients and their families. Throughout National Kidney Month, activities may include educational events, screenings, fundraisers, advocacy campaigns, and social media initiatives aimed at raising awareness and promoting kidney health. By participating in these activities and spreading the word about kidney health, individuals can help reduce the burden of kidney disease and improve outcomes for those affected by this condition.

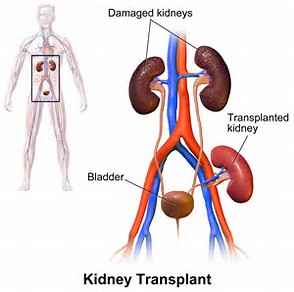
Donate Life Month is an observance held annually in April [Gail here: more on that next month] to raise awareness about organ donation and encourage individuals to register as organ, eye, and tissue donors. During Donate Life Month, various events, campaigns, and educational initiatives are organized by organizations such as Donate Life America, transplant centers, and other healthcare organizations to promote the importance of organ donation and transplantation. The primary goal of Donate Life Month is to inspire people to make the decision to become organ donors and to discuss their wishes with their families. By increasing awareness about the critical need for organ donors and dispelling myths and misconceptions surrounding donation, advocates hope to save more lives and improve the quality of life for individuals awaiting life-saving transplants. Throughout the month of April, activities may include community outreach events, educational workshops, social media campaigns, donor registration drives, and storytelling initiatives featuring transplant recipients, donor families, and healthcare professionals. These efforts aim to highlight the profound impact of organ donation on individuals and communities and to encourage meaningful conversations about donation and transplantation. Participation in Donate Life Month provides an opportunity for individuals to learn more about the donation process, the importance of registering as a donor, and the incredible gift of life that organ donation represents. By engaging with the Donate Life community and supporting initiatives to raise awareness, individuals can help to increase the number of registered donors and ultimately save more lives through organ transplantation.
Becoming a living kidney donor is a decision that carries significant weight, both for the donor and the recipient. Understanding the full spectrum of advantages and disadvantages associated with this altruistic act is essential for individuals contemplating such a profound gesture, particularly in light of the critical shortage of available kidneys for transplantation.

On the positive side, the primary benefit of being a living kidney donor lies in the opportunity to save a life. With approximately 100,000 individuals approved for kidney transplants in the United States alone, the demand for organ donors far exceeds the available supply. By offering one of their kidneys to someone suffering from kidney failure, donors directly impact the recipient’s health and lifespan. This act of selflessness not only saves a life but also brings immeasurable satisfaction and a deep sense of fulfillment to the donor, knowing they’ve made a tangible and potentially life-saving difference in another person’s life. Moreover, the impact of a kidney donation extends beyond the individual recipient to their family, friends, and community. It fosters a culture of compassion and generosity, inspiring others to consider organ donation as a means of giving back and making a positive impact on society. Additionally, undergoing the rigorous medical evaluation process before donation can lead to early detection and treatment of previously undiagnosed health issues in the donor, ensuring the best possible outcome for both parties involved. Furthermore, living kidney donors typically experience minimal long-term health effects, with studies indicating that they generally enjoy good health and life expectancy post-donation. This reassurance can alleviate concerns about the potential impact on the donor’s own health and well-being. Additionally, the experience of being a living kidney donor can lead to personal growth and a deeper appreciation for one’s own health. Donors often report feeling a renewed sense of purpose and gratitude for their own well-being, inspiring them to prioritize self-care and adopt healthier lifestyle habits.
However, despite the numerous benefits associated with being a living kidney donor, there are also potential drawbacks and considerations to be mindful of. Donating a kidney involves undergoing surgery, which carries inherent risks such as bleeding, infection, and adverse reactions to anesthesia. While serious complications are rare, donors must be prepared for the physical discomfort and recovery period following surgery, which may necessitate several weeks of rest and limited activity. Furthermore, the emotional and psychological impact of being a living kidney donor should not be underestimated. Donors may experience a range of emotions, including anxiety, guilt, and worry about the recipient’s well-being, as well as concerns about their own health and future. It is essential for donors to have access to adequate support and counseling throughout the donation process to address any emotional challenges and ensure their well-being. Additionally, there may be practical and logistical considerations to contend with, such as arranging time off from work for surgery and recovery, coordinating travel and accommodations if the donor and recipient are not in the same location, and navigating financial expenses related to the donation process. Donors should carefully plan and prepare for these logistical challenges to minimize stress and ensure a smooth donation experience.
In summary, while being a living kidney donor offers the opportunity to save a life and make a profound difference in someone’s life, it is essential for individuals to carefully weigh the potential risks and benefits before making this decision. By thoroughly considering all aspects of the donation process and seeking support from medical professionals and support networks, potential donors can make an informed decision that aligns with their values and priorities, ultimately contributing to the greater good and leaving a lasting legacy of compassion and generosity.
Thank you for closing out National Kidney Month and easing us into National Donate Life Month, Leesa.
Until next week,
Keep living your life!



























 Responsum for CKD does just that, but I’ll let them explain their app themselves. This is from their April 28th blog at
Responsum for CKD does just that, but I’ll let them explain their app themselves. This is from their April 28th blog at 
 About Responsum Health
About Responsum Health
 One such person is Steve L. Belcher. After I realized I’ve been seeing his name again and again on Facebook, I decided to ask him to guest blog. I certainly learned a lot from his blog and I hope you do, too. This is not a competition among Chronic Kidney Disease awareness advocates, but an informal coalition. We all want you to know as much as you can about this disease we share. Steve’s blog explains the background for all the shows he broadcasts. Kudos, my friend, kudos.
One such person is Steve L. Belcher. After I realized I’ve been seeing his name again and again on Facebook, I decided to ask him to guest blog. I certainly learned a lot from his blog and I hope you do, too. This is not a competition among Chronic Kidney Disease awareness advocates, but an informal coalition. We all want you to know as much as you can about this disease we share. Steve’s blog explains the background for all the shows he broadcasts. Kudos, my friend, kudos. President of Operations. During our early beginnings, we began broadcasting Urban Renal Talk with Tamika and Steve from our cellphones to our Facebook Page. The Urban Renal Talk with Tamika and Steve broadcast was created to interview kidney patients and professionals making a difference in the chronic kidney disease community. Since the beginning Urban Renal Talk with Tamika and Steve has come a long way with over four hundred broadcast shows to date. Our shows consist of digital broadcasting, which is the distribution of audio or video content to a dispersed audience via any electronic mass communication medium.
President of Operations. During our early beginnings, we began broadcasting Urban Renal Talk with Tamika and Steve from our cellphones to our Facebook Page. The Urban Renal Talk with Tamika and Steve broadcast was created to interview kidney patients and professionals making a difference in the chronic kidney disease community. Since the beginning Urban Renal Talk with Tamika and Steve has come a long way with over four hundred broadcast shows to date. Our shows consist of digital broadcasting, which is the distribution of audio or video content to a dispersed audience via any electronic mass communication medium.

 Last week, I promised to write about COVID-19 and Chronic Kidney Disease for today’s blog. This topic has touched me personally since one of my daughters was sent to the hospital when it was suspected she’d contacted the virus. Without the COVID-19 test, we still don’t know if she has the virus. We do know she still has the cough. Luckily, an x-ray proved her lungs were clear, so she was sent home with a Z-pack and orders to take Tylenol. No, she doesn’t have CKD, but her treatment at the hospital left me with a lot of questions for those of us who do.
Last week, I promised to write about COVID-19 and Chronic Kidney Disease for today’s blog. This topic has touched me personally since one of my daughters was sent to the hospital when it was suspected she’d contacted the virus. Without the COVID-19 test, we still don’t know if she has the virus. We do know she still has the cough. Luckily, an x-ray proved her lungs were clear, so she was sent home with a Z-pack and orders to take Tylenol. No, she doesn’t have CKD, but her treatment at the hospital left me with a lot of questions for those of us who do.
 https://www.prevention.com/health/a31245792/coronavirus-high-risk-groups/
https://www.prevention.com/health/a31245792/coronavirus-high-risk-groups/



 I think we’re ready for Dax’s guest blog now.
I think we’re ready for Dax’s guest blog now.
 I enrolled back in school and finished my 6 credits finally achieving my degree. During this time the world began to change. More and more negativity seemed to be seeping into my life and I found myself in a negative space despite having everything I wanted. I needed to make a change. At the end of 2017 I committed to being positive, uplifting and to helping others the way I can. I started making videos while I was actually on dialysis just to let others know that they were not alone and that they needed to continue their fight.
I enrolled back in school and finished my 6 credits finally achieving my degree. During this time the world began to change. More and more negativity seemed to be seeping into my life and I found myself in a negative space despite having everything I wanted. I needed to make a change. At the end of 2017 I committed to being positive, uplifting and to helping others the way I can. I started making videos while I was actually on dialysis just to let others know that they were not alone and that they needed to continue their fight.

 “Sensory information about motion, equilibrium, and spatial orientation is provided by the vestibular apparatus, which in each ear includes the utricle, saccule, and three semicircular canals. The utricle and saccule detect gravity (information in a vertical orientation) and linear movement. The semicircular canals, which detect rotational movement, are located at right angles to each other and are filled with a fluid called endolymph. When the head rotates in the direction sensed by a particular canal, the endolymphatic fluid within it lags behind because of inertia, and exerts pressure against the canal’s sensory receptor. The receptor then sends impulses to the brain about movement from the specific canal that is stimulated. When the vestibular organs on both sides of the head are functioning properly, they send symmetrical impulses to the brain. (Impulses originating from the right side are consistent with impulses originating from the left side.)”
“Sensory information about motion, equilibrium, and spatial orientation is provided by the vestibular apparatus, which in each ear includes the utricle, saccule, and three semicircular canals. The utricle and saccule detect gravity (information in a vertical orientation) and linear movement. The semicircular canals, which detect rotational movement, are located at right angles to each other and are filled with a fluid called endolymph. When the head rotates in the direction sensed by a particular canal, the endolymphatic fluid within it lags behind because of inertia, and exerts pressure against the canal’s sensory receptor. The receptor then sends impulses to the brain about movement from the specific canal that is stimulated. When the vestibular organs on both sides of the head are functioning properly, they send symmetrical impulses to the brain. (Impulses originating from the right side are consistent with impulses originating from the left side.)”
 It’s the last few days of 2019 and this year has whizzed by. My dance with pancreatic cancer has been a trip I could have done without, but the birth of my grandson more than made up for it. Now I get to see him all the time and I only have one more regiment of chemotherapy to go.
It’s the last few days of 2019 and this year has whizzed by. My dance with pancreatic cancer has been a trip I could have done without, but the birth of my grandson more than made up for it. Now I get to see him all the time and I only have one more regiment of chemotherapy to go. The words were written by Scottish poet Robert Burns in 1788, but Burns himself revealed at the time of composing it that he had collected the words after listening to the verse of an old man on his travels, claiming that his version of ‘Auld Lang Syne’ marked the first time it had been formally written down.
The words were written by Scottish poet Robert Burns in 1788, but Burns himself revealed at the time of composing it that he had collected the words after listening to the verse of an old man on his travels, claiming that his version of ‘Auld Lang Syne’ marked the first time it had been formally written down. “Specifically, the legislation does the following:
“Specifically, the legislation does the following: In case you haven’t heard yet, my youngest and her husband are having a little boy at the end of the month. I’ve noticed that, as millennials, their generation shares what they already have instead of running out to buy new as my generation – the baby boomers – did. One thing that was shared with them was a 16 year old crib in ace condition.
In case you haven’t heard yet, my youngest and her husband are having a little boy at the end of the month. I’ve noticed that, as millennials, their generation shares what they already have instead of running out to buy new as my generation – the baby boomers – did. One thing that was shared with them was a 16 year old crib in ace condition.
 “The first step in treating lead poisoning is to remove the source of the contamination. If you can’t remove lead from your environment, you might be able to reduce the likelihood that it will cause problems. For instance, sometimes it’s better to seal in rather than remove old lead paint. Your local health department can recommend ways to identify and reduce lead in your home and community. For children and adults with relatively low lead levels, simply avoiding exposure to lead might be enough to reduce blood lead levels.
“The first step in treating lead poisoning is to remove the source of the contamination. If you can’t remove lead from your environment, you might be able to reduce the likelihood that it will cause problems. For instance, sometimes it’s better to seal in rather than remove old lead paint. Your local health department can recommend ways to identify and reduce lead in your home and community. For children and adults with relatively low lead levels, simply avoiding exposure to lead might be enough to reduce blood lead levels. I like my dentist, especially when he tells me something I didn’t know. When I went to see him last time, I told him my chemo experience and how dry my mouth was. I thought they might be related. He patiently gave me the same information as the Mayo Clinic at
I like my dentist, especially when he tells me something I didn’t know. When I went to see him last time, I told him my chemo experience and how dry my mouth was. I thought they might be related. He patiently gave me the same information as the Mayo Clinic at 

 “Common symptoms include:
“Common symptoms include: Let’s go to my favorite dictionary, the Merriam-Webster Dictionary at
Let’s go to my favorite dictionary, the Merriam-Webster Dictionary at 













 Not part of my bag of tricks – I mean therapy toys – is the foot roller. This is another therapy toy I bought on Amazon after trying one out at an occupational therapy treatment. Have you ever heard the expression ‘hurts so good?’ That’s what this feels like while you roll it back and forth under your feet. Lest you get me wrong, it does not hurt enough to make you want to stop, just enough to make those tingly feet tingle even more.
Not part of my bag of tricks – I mean therapy toys – is the foot roller. This is another therapy toy I bought on Amazon after trying one out at an occupational therapy treatment. Have you ever heard the expression ‘hurts so good?’ That’s what this feels like while you roll it back and forth under your feet. Lest you get me wrong, it does not hurt enough to make you want to stop, just enough to make those tingly feet tingle even more.
 “Healthy kidneys remove extra fluid and waste from your blood, but let proteins and other important nutrients pass through and return to your blood stream. When your kidneys are not working as well as they should, they can let some protein (albumin) escape through their filters, into your urine. When you have protein in your urine, it is called proteinuria (or albuminuria). Having protein in your urine can be a sign of nephrotic syndrome, or an early sign of kidney disease.”
“Healthy kidneys remove extra fluid and waste from your blood, but let proteins and other important nutrients pass through and return to your blood stream. When your kidneys are not working as well as they should, they can let some protein (albumin) escape through their filters, into your urine. When you have protein in your urine, it is called proteinuria (or albuminuria). Having protein in your urine can be a sign of nephrotic syndrome, or an early sign of kidney disease.”
 I was also given physical exercises to do, like raising my fisted hands above my head and straightening out my fist several times. This is one of many exercises. Do you remember the old TV show, E.R? It takes me slightly longer than one 43 minute episode to complete the exercises.
I was also given physical exercises to do, like raising my fisted hands above my head and straightening out my fist several times. This is one of many exercises. Do you remember the old TV show, E.R? It takes me slightly longer than one 43 minute episode to complete the exercises.




 HERE’S THE STORY
HERE’S THE STORY
 What does CKD research typically focus on?
What does CKD research typically focus on? 
 Thank you to Dr. Seuss for lending us the title of today’s blog. Oh, you haven’t heard of him yet? According to Encyclopaedia Britannica at
Thank you to Dr. Seuss for lending us the title of today’s blog. Oh, you haven’t heard of him yet? According to Encyclopaedia Britannica at 
 By visiting booknowmed.com you will be able to browse more than 450 dialysis centers in 380 destinations, across five continents. This includes standard holiday options like Spain, Greece, and Turkey, as well some less ordinary destinations like Bali, Sri Lanka, Miami, Brazil and Argentina. Cuba, Barbados, and Curacao are coming up this month.
By visiting booknowmed.com you will be able to browse more than 450 dialysis centers in 380 destinations, across five continents. This includes standard holiday options like Spain, Greece, and Turkey, as well some less ordinary destinations like Bali, Sri Lanka, Miami, Brazil and Argentina. Cuba, Barbados, and Curacao are coming up this month.
 Ms. Rae-Garwood’s writing started out as a means to an end for a single parent with two children and a need for more income than her career as a NYC teacher afforded. Gail retired from both college teaching and acting – after a bit of soul searching about where her CKD limited energy would be best spent – early in 2013. Since her diagnose, Ms. Rae-Garwood writes most often about Chronic Kidney Disease, although she does write fiction. She has a three time award winning weekly blog (Surprise!) about this topic at
Ms. Rae-Garwood’s writing started out as a means to an end for a single parent with two children and a need for more income than her career as a NYC teacher afforded. Gail retired from both college teaching and acting – after a bit of soul searching about where her CKD limited energy would be best spent – early in 2013. Since her diagnose, Ms. Rae-Garwood writes most often about Chronic Kidney Disease, although she does write fiction. She has a three time award winning weekly blog (Surprise!) about this topic at 



 While there are numerous objectives for this year’s World Kidney Day, the one that lays closest to my heart is this one: ‘Encourage systematic screening of all patients with diabetes and hypertension for CKD.’
While there are numerous objectives for this year’s World Kidney Day, the one that lays closest to my heart is this one: ‘Encourage systematic screening of all patients with diabetes and hypertension for CKD.’

 That, of course, prompted me to go directly to the National Kidney Foundation’s information about National Kidney Month at
That, of course, prompted me to go directly to the National Kidney Foundation’s information about National Kidney Month at  I wanted to share this quote from the AKF with you, both as a CKD awareness advocate and a woman:
I wanted to share this quote from the AKF with you, both as a CKD awareness advocate and a woman: Her question? It’s about fiber and Chronic Kidney Disease. But first, let’s find out exactly what fiber is. According to Harvard’s T. H. Chan School of Public Health at
Her question? It’s about fiber and Chronic Kidney Disease. But first, let’s find out exactly what fiber is. According to Harvard’s T. H. Chan School of Public Health at
 ingredients and found this:
ingredients and found this:
 levels in high-altitude areas can add to anxiety symptoms.
levels in high-altitude areas can add to anxiety symptoms.
 Clinic at
Clinic at 
 Now think about it another way: you already have a compromised immune system because you have CKD. Gallstones can cause infection of the gallbladder. As in Nima’s experience, infection causes white blood cell elevation. So you know you have an infection, you might even realize it could be in the bile ducts, too. But did you check to see if there’s infection in other areas of your body? That would mean you can read your own test results or have the kind of relationship with your doctors – especially your nephrologist – to freely ask questions.
Now think about it another way: you already have a compromised immune system because you have CKD. Gallstones can cause infection of the gallbladder. As in Nima’s experience, infection causes white blood cell elevation. So you know you have an infection, you might even realize it could be in the bile ducts, too. But did you check to see if there’s infection in other areas of your body? That would mean you can read your own test results or have the kind of relationship with your doctors – especially your nephrologist – to freely ask questions. I had trouble with this idea at first, thinking it selfish when it was my husband who needed help – not me. I was wrong. The Mayo Clinic at
I had trouble with this idea at first, thinking it selfish when it was my husband who needed help – not me. I was wrong. The Mayo Clinic at 

 the symptoms. These are the same whether you’re the patient or the caretaker. I happen to be both a CKD patient and my Alzheimer’s husband’s caretaker, although we call me his care partner as suggested by the Alzheimer’s Association.
the symptoms. These are the same whether you’re the patient or the caretaker. I happen to be both a CKD patient and my Alzheimer’s husband’s caretaker, although we call me his care partner as suggested by the Alzheimer’s Association. Today is the last day of the eight day Chanukah celebration for us and all of you who celebrate this holiday. We usually throw a blowout party for anywhere from 30 to 50 people. But just a couple of months ago, we hosted a blowout pre-wedding potluck party for my daughter and her fiancé … and it was wonderful. Yet, it was clear that we can no longer handle undertaking such large parties. I had expressed my doubts last year about how long we’d be able to keep up the Chanukah party.
Today is the last day of the eight day Chanukah celebration for us and all of you who celebrate this holiday. We usually throw a blowout party for anywhere from 30 to 50 people. But just a couple of months ago, we hosted a blowout pre-wedding potluck party for my daughter and her fiancé … and it was wonderful. Yet, it was clear that we can no longer handle undertaking such large parties. I had expressed my doubts last year about how long we’d be able to keep up the Chanukah party.
 I hesitated to ask Steve to guest blog since, at the time, I was only writing about Chronic Kidney Disease. Since then, readers have asked me to write about all sorts of topics dealing with the kidneys, not just CKD. So I did. Steve and his thoughts on being a transplant fit right in to this new agenda. When I did ask him to guest blog, I received a return response that was one of the most gracious acceptances… and they’ve all been gracious. I’ll turn the blog over to Steve Winfree now.
I hesitated to ask Steve to guest blog since, at the time, I was only writing about Chronic Kidney Disease. Since then, readers have asked me to write about all sorts of topics dealing with the kidneys, not just CKD. So I did. Steve and his thoughts on being a transplant fit right in to this new agenda. When I did ask him to guest blog, I received a return response that was one of the most gracious acceptances… and they’ve all been gracious. I’ll turn the blog over to Steve Winfree now.
 By now it shouldn’t surprise me that as I’m out and about I’m constantly meeting more and more people with a connection to kidney disease. That was not the case 21 years ago, or even four years ago for that matter. What changed? The opening of my eyes to statistics I was previously unaware of, and frankly I found to be quite shocking and unacceptable. I’ll get to those stats a little later.
By now it shouldn’t surprise me that as I’m out and about I’m constantly meeting more and more people with a connection to kidney disease. That was not the case 21 years ago, or even four years ago for that matter. What changed? The opening of my eyes to statistics I was previously unaware of, and frankly I found to be quite shocking and unacceptable. I’ll get to those stats a little later.
 kidneys failed! He and his dance partner and instructor, Brianna Santiago, spent six months of grueling practices preparing for their energetic performance to Pharrell William’s song Happy, demonstrating the improved quality of life home dialysis can provide, and that dialysis does not have to be a death sentence.
kidneys failed! He and his dance partner and instructor, Brianna Santiago, spent six months of grueling practices preparing for their energetic performance to Pharrell William’s song Happy, demonstrating the improved quality of life home dialysis can provide, and that dialysis does not have to be a death sentence. University of Arizona
University of Arizona  Chronic Kidney Disease awareness advocates have a tendency to hang out together online. One who has become a good buddy and happens to live in Hawaii (Now you see why we’re online buddies.), and I were going back and forth about how it’s important to be what I call a lifelong learner. To put it another way, someone who investigates that about which they don’t know. The timing was good.
Chronic Kidney Disease awareness advocates have a tendency to hang out together online. One who has become a good buddy and happens to live in Hawaii (Now you see why we’re online buddies.), and I were going back and forth about how it’s important to be what I call a lifelong learner. To put it another way, someone who investigates that about which they don’t know. The timing was good. , they can include:
, they can include: an electrocardiogram
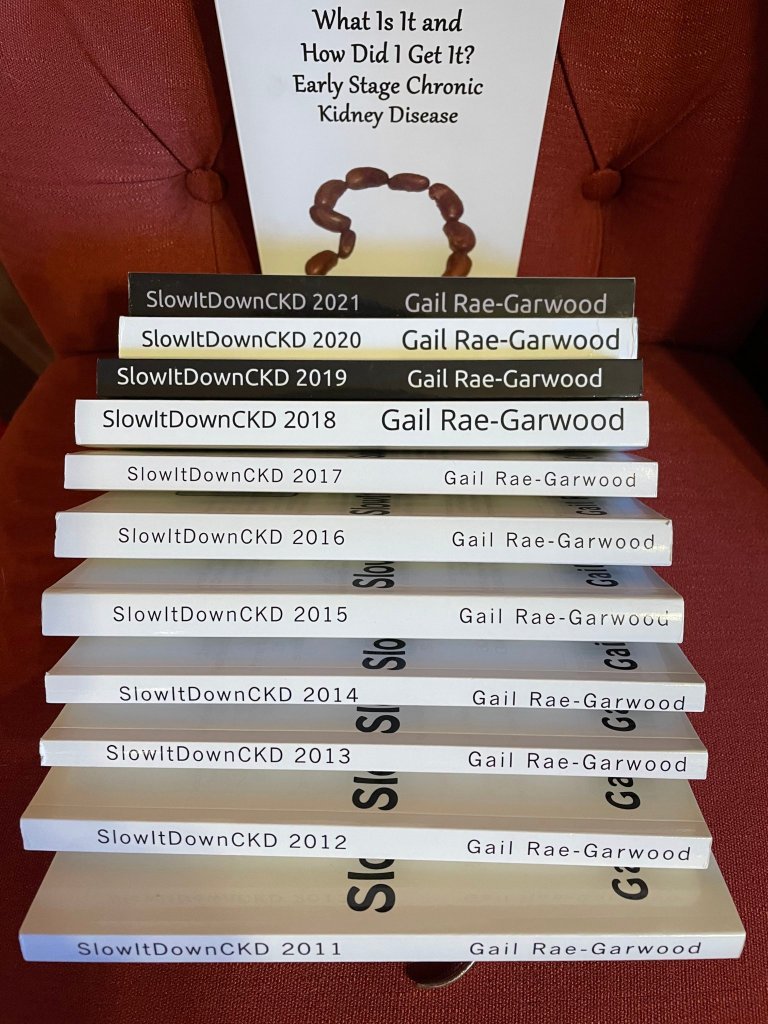
an electrocardiogram Some people think SlowItDownCKD is a business; it’s not. Some think it’s a profit maker; it’s not. So, what is it you ask? It’s a vehicle for spreading awareness of Chronic Kidney Disease and whatever goes along with the disease. Why do I do it? Because I had no idea what it was, nor how I might have prevented the disease, nor how to deal with it effectively once I was diagnosed.
Some people think SlowItDownCKD is a business; it’s not. Some think it’s a profit maker; it’s not. So, what is it you ask? It’s a vehicle for spreading awareness of Chronic Kidney Disease and whatever goes along with the disease. Why do I do it? Because I had no idea what it was, nor how I might have prevented the disease, nor how to deal with it effectively once I was diagnosed.
 That, of course, brings us to the Facebook support groups. I miss my New York daughter and she misses me, so we sometimes have coffee together separately. She has a cup of coffee and I do at the same time. It’s not like being together in person, but it’s something. You can find support the same way via Facebook. Since I’m both running out of room and have periodically reviewed these groups, I’m just going to list a few. You can use the search bar at the top of your Facebook page for others.
That, of course, brings us to the Facebook support groups. I miss my New York daughter and she misses me, so we sometimes have coffee together separately. She has a cup of coffee and I do at the same time. It’s not like being together in person, but it’s something. You can find support the same way via Facebook. Since I’m both running out of room and have periodically reviewed these groups, I’m just going to list a few. You can use the search bar at the top of your Facebook page for others.
 okay, I guess that sort of makes sense. And then, oh my, I developed diabetes. But how? I’d never questioned how that worked before, but I certainly did now.
okay, I guess that sort of makes sense. And then, oh my, I developed diabetes. But how? I’d never questioned how that worked before, but I certainly did now. Guilty on all three counts as far as symptoms. It gets worse. I uncovered this fact in
Guilty on all three counts as far as symptoms. It gets worse. I uncovered this fact in  I would say I’m heart… uh, kidney…broken about this development, but the truth is I’m not. I don’t like it; I don’t want it, but I can do something about it. I’d already cut out complex carbs and sugar laden foods in an abortive attempt to lose weight for my health. Well, maybe my daughter’s wedding on October 6th had something to do with that decision, too.
I would say I’m heart… uh, kidney…broken about this development, but the truth is I’m not. I don’t like it; I don’t want it, but I can do something about it. I’d already cut out complex carbs and sugar laden foods in an abortive attempt to lose weight for my health. Well, maybe my daughter’s wedding on October 6th had something to do with that decision, too. That began the journey to today, a journey that began on March 3rd, 2016, when The Forever is Tomorrow Foundation was officially launched. The foundation is committed to raising awareness and shedding light on kidney disease through the creation of video content distributed via the web and social media. With many hopes and plans for the future, we are pushing forward as time and funds are available to create new content and keep things moving.
That began the journey to today, a journey that began on March 3rd, 2016, when The Forever is Tomorrow Foundation was officially launched. The foundation is committed to raising awareness and shedding light on kidney disease through the creation of video content distributed via the web and social media. With many hopes and plans for the future, we are pushing forward as time and funds are available to create new content and keep things moving.
 In some ways, I live the typical middle class American mom life. I have a middle schooler and a high schooler. I work from home, my husband works a 9-5 in an office. The kids go to school, do their homework, go to activities. I have coffee dates with friends and dinner out with family, we go to the movies, we stay home and do yard work. Same routine, same rhythm as so many other families we know.
In some ways, I live the typical middle class American mom life. I have a middle schooler and a high schooler. I work from home, my husband works a 9-5 in an office. The kids go to school, do their homework, go to activities. I have coffee dates with friends and dinner out with family, we go to the movies, we stay home and do yard work. Same routine, same rhythm as so many other families we know.

 Our organization works with people to ensure that they are being treated fairly in the school system, read more in one patient’s story
Our organization works with people to ensure that they are being treated fairly in the school system, read more in one patient’s story 

 suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference.
suggesting I do so for years, but I’m not a joiner. Let’s change that; I wasn’t a joiner. The AAKP conference made the difference. AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”
AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”
 Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at
Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at  American Kidney Fund
American Kidney Fund  That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible.
That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible. pretty quickly, too. But then I noticed that I was hungry pretty much only after I ate.
pretty quickly, too. But then I noticed that I was hungry pretty much only after I ate.
 According the renal diet I follow, the Northern Arizona Council on Renal Nutrition Diet, I could eat all of these foods. According to my food sensitivities, I could only eat oatmeal, some fruits, and vegetables. Maybe that’s why eating makes me hungry.
According the renal diet I follow, the Northern Arizona Council on Renal Nutrition Diet, I could eat all of these foods. According to my food sensitivities, I could only eat oatmeal, some fruits, and vegetables. Maybe that’s why eating makes me hungry.

 ICD-10-CM Diagnosis Code C90.01
ICD-10-CM Diagnosis Code C90.01


 “Then I found this in BrightHub.com’s February 13th article The Importance of the Potassium and Sodium Balance.
“Then I found this in BrightHub.com’s February 13th article The Importance of the Potassium and Sodium Balance.
 Will she need extra medicines when she’s pregnant? Women trying to get pregnant should start taking the vitamin folic acid to reduce the chance of their baby having spina bifida, an abnormality of the spinal cord. The normal dose of folic acid is 400ug per day and can be bought over the counter. However, if the folate level is low or a patient is on the drug azathioprine which affects the way folic acid works, the dose of 5mg daily may be prescribed. No other over the counter vitamins are required unless specifically advised by a doctor or midwife. All pregnant patients should avoid additional supplements of vitamin A. If vitamin D levels are low GPs will advise correction with high dose prescribed vitamin D (also known as cholecalciferol). Women with kidney diseases are at higher risk of pre-eclampsia. Aspirin lowers the risk of pre eclampsia, and women with CKD are usually offered a low dose aspirin (75mg once daily) throughout pregnancy unless there are specific reasons not to take it e.g. they are allergic to aspirin. Pregnant women with a high level of protein in their urine have an increased risk of developing blood clots (thrombosis). This can be reduced by small daily injections of low molecular weight heparin. Heparin reduces the way the blood clots. Both pregnancy and CKD can cause a low blood count (
Will she need extra medicines when she’s pregnant? Women trying to get pregnant should start taking the vitamin folic acid to reduce the chance of their baby having spina bifida, an abnormality of the spinal cord. The normal dose of folic acid is 400ug per day and can be bought over the counter. However, if the folate level is low or a patient is on the drug azathioprine which affects the way folic acid works, the dose of 5mg daily may be prescribed. No other over the counter vitamins are required unless specifically advised by a doctor or midwife. All pregnant patients should avoid additional supplements of vitamin A. If vitamin D levels are low GPs will advise correction with high dose prescribed vitamin D (also known as cholecalciferol). Women with kidney diseases are at higher risk of pre-eclampsia. Aspirin lowers the risk of pre eclampsia, and women with CKD are usually offered a low dose aspirin (75mg once daily) throughout pregnancy unless there are specific reasons not to take it e.g. they are allergic to aspirin. Pregnant women with a high level of protein in their urine have an increased risk of developing blood clots (thrombosis). This can be reduced by small daily injections of low molecular weight heparin. Heparin reduces the way the blood clots. Both pregnancy and CKD can cause a low blood count ( Oh, clone… as in Dolly, the sheep back in Scotland in 1995. Got it.
Oh, clone… as in Dolly, the sheep back in Scotland in 1995. Got it.




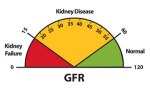
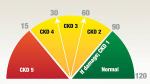 decline in our kidney function. I maintain that if only my primary care physician had told me when he first noticed that 39% GFR, maybe I wouldn’t be in stage 3 of 5. Maybe those now on dialysis or searching for a transplant wouldn’t be in the position they are, either.
decline in our kidney function. I maintain that if only my primary care physician had told me when he first noticed that 39% GFR, maybe I wouldn’t be in stage 3 of 5. Maybe those now on dialysis or searching for a transplant wouldn’t be in the position they are, either.
 The literature suggests early nephrologist involvement improves long-term outcomes. Proactive primary care offers longitudinal guidance for making the enormous lifestyle changes in diet, exercise, stress management, hydration, sleep and toxic exposures, while offering psychological counseling that is required to achieve such changes. The cross-over benefits for patients’ other diagnoses is well known.
The literature suggests early nephrologist involvement improves long-term outcomes. Proactive primary care offers longitudinal guidance for making the enormous lifestyle changes in diet, exercise, stress management, hydration, sleep and toxic exposures, while offering psychological counseling that is required to achieve such changes. The cross-over benefits for patients’ other diagnoses is well known. Welcome to the last blog of National Kidney Month 2018. We all know I rarely write about dialysis or transplant, but a friend who is awaiting a transplant brought this book to my attention. This particular section of the book sparked my interest since non-compliance can be an issue in any stage of kidney disease. One part of my mission is to create awareness among Chronic Kidney Disease patients, their friends, families, and loved ones of how important compliance with their medical team is. Dr. Michael B. Fisher is a nephrologist who thinks the same way.
Welcome to the last blog of National Kidney Month 2018. We all know I rarely write about dialysis or transplant, but a friend who is awaiting a transplant brought this book to my attention. This particular section of the book sparked my interest since non-compliance can be an issue in any stage of kidney disease. One part of my mission is to create awareness among Chronic Kidney Disease patients, their friends, families, and loved ones of how important compliance with their medical team is. Dr. Michael B. Fisher is a nephrologist who thinks the same way.



