A very active reader – who happens to be a transplantee – asked me to write about spilling protein. As a CKD patient, I’ve never been told I was doing that. However, one of my daughters was told she was spilling urine. She does not have chronic kidney disease. Hmmm.

Way back in 2020, I became interested in proteinuria simply because, while I knew the meaning of the word, I didn’t really know what the definition meant. In other words, I could break down the parts of the word [protein and urine] but didn’t get what they meant when combined. I found this information from The Mayo Clinic useful in helping me to understand:
“Protein in urine — known as proteinuria (pro-tee-NU-ree-uh) — is excess protein found in a urine sample. Protein is one of the substances identified during a test to analyze the content of your urine (urinalysis).
Low levels of protein in urine are normal. Temporarily high levels of protein in urine aren’t unusual either, particularly in younger people after exercise or during an illness.
Persistently high levels of protein in urine may be a sign of kidney disease.”
Oh, maybe this explained why my daughter was spilling protein into her urine. Perhaps she was ill or had just exercised before the test not realizing that would affect the results.
I wondered precisely what it was that healthy kidneys did do. The American Kidney Fund explained a bit more:
“Healthy kidneys remove extra fluid and waste from your blood, but let proteins and other important nutrients pass through and return to your blood stream. When your kidneys are not working as well as they should, they can let some protein (albumin) escape through their filters, into your urine. When you have protein in your urine, it is called proteinuria …. Having protein in your urine can be a sign of nephrotic syndrome, or an early sign of kidney disease.”
There’s another reason you don’t want to have proteinuria as WebMD clarifies:
“Protein is an important component of every cell in the body. Hair and nails are mostly made of protein. Your body uses protein to build and repair tissues. You also use protein to make enzymes, hormones, and other body chemicals. Protein is an important building block of bones, muscles, cartilage, skin, and blood.”
I thought I’d throw this tidbit in since I just spent two weeks writing about biopsies. The paper Patient education: Kidney (renal) biopsy (Beyond the Basics) written by William L Whittier, MD, FASN and Stephen M Korbet, MD, MACP published on UpToDate informs us:
““The following are the most common reasons for kidney biopsy. You may have one or more of these problems, but not everyone with these problems needs a kidney biopsy:
●Blood in the urine (called hematuria). …
●Protein in the urine (called proteinuria) – This occurs in many people with kidney problems. A kidney biopsy may be recommended if you have high or increasing levels of protein in the urine or if you have proteinuria along with other signs of kidney disease….
●Problems with kidney function – If your kidneys suddenly or slowly stop functioning normally, a kidney biopsy may be recommended, especially if the cause of your kidney problem is unclear.”
Take a look at the second reason for having a biopsy.

I think it would make sense to learn how the kidney becomes so damaged that it allows protein, which is meant to return to the blood, to spill into the urine. I turned to the Cleveland Clinic to find out:
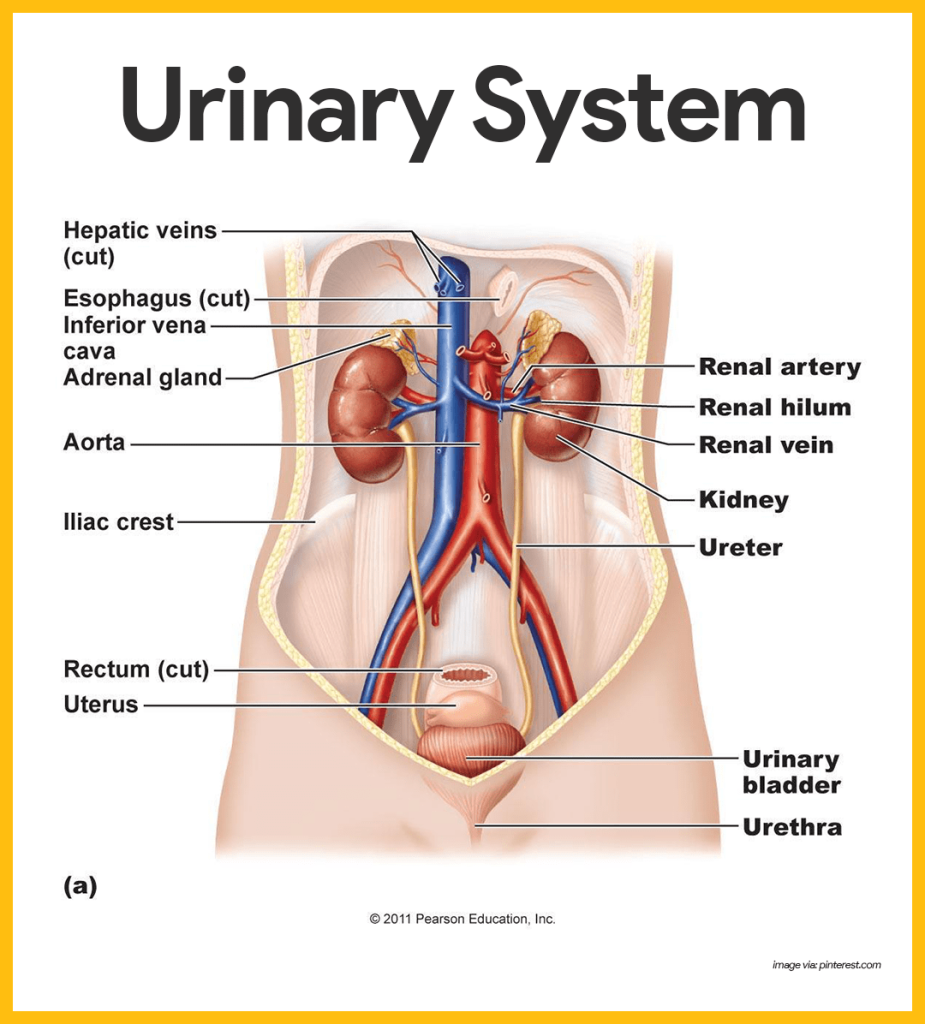
“Protein gets into the urine if the kidneys aren’t working properly. Normally, glomeruli, which are tiny loops of capillaries (blood vessels) in the kidneys, filter waste products and excess water from the blood.
Glomeruli pass these substances, but not larger proteins and blood cells, into the urine. If smaller proteins sneak through the glomeruli, tubules (long, thin, hollow tubes in the kidneys) recapture those proteins and keep them in the body.
However, if the glomeruli or tubules are damaged, if there is a problem with the reabsorption process of the proteins, or if there is an excessive protein load, the proteins will flow into the urine.”
‘Excessive protein load’ That’s why our protein intake is limited. We do not want to overwork and possibly damage our kidneys by relying on a diet of burgers, chicken, steak, and salmon. This doesn’t mean you cannot have these or similar foods; simply that you need to limit them each day. Your nephrologist or renal dietitian will tell you how much protein per day is the right amount for you.
I wondered if that was the only cause of damaged kidneys. According to the Mayo Clinic, it’s not. There’s also:

- “Type 1 or type 2 diabetes
- High blood pressure
- Glomerulonephritis (gloe-mer-u-low-nuh-FRY-tis), an inflammation of the kidney’s filtering units (glomeruli)
- Interstitial nephritis (in-tur-STISH-ul nuh-FRY-tis), an inflammation of the kidney’s tubules and surrounding structures
- Polycystic kidney disease or other inherited kidney diseases
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers
- Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux, a condition that causes urine to back up into your kidneys
- Recurrent kidney infection, also called pyelonephritis (pie-uh-low-nuh-FRY-tis)”
Remember, CKD is at least three months of your kidney function declining.
Since the question was asked by a transplantee, let’s see if there’s anything to add specifically for this group of people. New York based Nao Medical made it easy to understand:
“There are several factors that can contribute to the development of proteinuria in kidney transplant patients. These include:
- Rejection of the transplanted kidney
- Infection
- Medications
- High blood pressure
- Diabetes”
Transplantees: Take note that rejection is not the only cause of proteinuria.

As for the treatment of proteinuria in transplantees, I am confused. I found research that stated Vitamin D would do the trick, others that recommended statins, and still other that said antihypertension drugs would help. I remind you that I am not a doctor and have never claimed to be one. In other words, speak with your nephrologist to discover which treatment is the best for your proteinuria.
I learned quite a bit today and hope you did, too.
Until next week,
Keep living your life!