As I was sitting in my allergist’s office last week, I started to wonder if Chronic Kidney Disease had anything to do with my runny nose. I’d thought it was the usual seasonal allergies, but over the last dozen years or so I’ve learned that almost every malady I experience has some kind of relation to my kidneys… so why not the runny nose?

The American Kidney Fund at https://bit.ly/3kvpjb9 explains for us:
“Granulomatosis with polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a disease that causes swelling and irritation of blood vessels in the kidneys, nose, sinuses, throat and lungs. Swollen blood vessels make it harder for blood to get to the organs and tissues that need it, which can be harmful. The disease also causes lumps called granulomas to form and damage the area around them. In some people GPA only affects the lungs. GPA that affects the kidneys can lead to chronic kidney disease and kidney failure.”
Whoa! Not good. Let’s see how it’s treated. The Cleveland Clinic at https://cle.clinic/3mjudss tells us,
“People with GPA who have critical organ system involvement are generally treated with corticosteroids [Gail here: commonly just called steroids] combined with another immunosuppressive medication such as cyclophosphamide (Cytoxan ®) or rituximab (Rituxan®). In patients who have less severe GPA, corticosteroids and methotrexate can be used initially. The goal of treatment is to stop all injury that is occurring as a result of GPA. If disease activity can be completely ‘turned off,’ this is called ‘remission.’ Once it is apparent that the disease is improving, doctors slowly reduce the corticosteroid dose and eventually hope to discontinue it completely. When cyclophosphamide is used, it is only given until the time of remission (usually around 3 to 6 months), after which time it is switched to another immunosuppressive agent, such as methotrexate, azathioprine (Imuran®), or mycophenolate mofetil (Cellcept®) to maintain remission. The treatment duration of the maintenance immunosuppressive medication may vary between individuals. In most instances, it is given for a minimum of 2 years before consideration is given to slowly reduce the dose toward discontinuation.”
If this sounds familiar, you’re right. It’s straight out of this year’s May 25th blog. Aha! Now we see the value of using the category drop down to the right of the blog.

Anyway, while this is interesting (to me, at least), it’s not answering my question: Can CKD cause sinus problems. What was that? You want to know what a runny nose has to do with your sinuses? Let’s find out.
I returned to the ever-reliable Cleveland Clinic, this time at https://cle.clinic/2FXOm7Q, for some information:
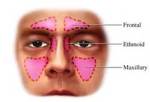
“Sinusitis is an inflammation, or swelling, of the tissue lining the sinuses. The sinuses are four paired cavities (spaces) in the head. They are connected by narrow channels. The sinuses make thin mucus that drains out of the channels of the nose. This drainage helps keep the nose clean and free of bacteria. Normally filled with air, the sinuses can get blocked and filled with fluid. When that happens, bacteria can grow and cause an infection (bacterial sinusitis).
This is also called rhinosinusitis, with ‘rhino’ meaning ‘nose.’ The nasal tissue is almost always swollen if sinus tissue is inflamed.”
It seems that you need a runny nose to avoid sinusitis. Is that right? I don’t think so, and neither does MedicineNet at https://www.medicinenet.com/sinusitis/article.htm.
“Sinusitis signs and symptoms include
sinus headache,
facial tenderness,
pressure or pain in the sinuses, in the ears and teeth,
fever,
cloudy discolored nasal or postnasal drainage, [I bolded this symptom.]
feeling of nasal stuffiness,
sore throat,
cough, and
occasionally facial swelling.”
So, now it seems that a runny nose can be a symptom of sinusitis.

And how does that fit in with having CKD? Before we answer that, I think we need to straighten out the differences between allergy and cold symptoms since both conditions may cause sinusitis.
“The symptoms of allergies and sinusitis overlap a lot. Both can give you a stuffy nose. If it’s allergies, you may also have:
Runny nose and sneezing
Watery or itchy eyes
Wheezing
If it’s sinusitis, besides a stuffy nose, you may have:
Thick, colored mucus
Painful, swollen feeling around your forehead, eyes, and cheeks
Headache or pain in your teeth
Post-nasal drip (mucus that moves from the back of your nose into your throat)
Bad breath
Cough and sore throat
Fatigue
Light fever”
Thank you to WebMD at https://www.webmd.com/allergies/sinusitis-or-allergies for the list above.
On to my original question. This is from Vick’s at https://vicks.com/en-us/treatments/how-to-treat-a-cold/how-to-stop-a-runny-nose. (Who better to go to than a trusted friend since childhood?)
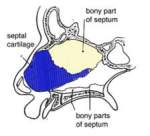
“A runny nose is a discharge of mucus from the nostrils. It’s the result of excess nasal mucus production. The excess nasal mucus leads to watery nasal secretions that flow out of your nostrils or drip down into your throat. A runny nose is a discharge of mucus from the nostrils. It’s the result of excess nasal mucus production. The excess nasal mucus leads to watery nasal secretions that flow out of your nostrils or drip down into your throat. Nasal congestion is due to the inflammation of the linings of the nasal cavity.”
Did you notice the word “inflammation” in the last sentence? Ahem, an article by Oleh M Akchurin of Weill Cornell Medical College and Frederick J Kaskel of Albert Einstein College of Medicine published by ResearchGate at https://bit.ly/3jtVzKL states:
“Chronic inflammation should be regarded as a common comorbid condition in CKD and especially in dialysis patients.”

And there you have it. Your (and my) runny nose can be caused – in part – from having CKD. Inflammation is the name of the game if you have Chronic Kidney Disease.
Although, in these times, I wonder if Covid-19 might somehow be involved in certain cases. Just remember, I’m not a doctor and never claimed to be one, so this just might be a question for your medical provider.
Until next week,
Keep living your life! (Safely: mask up, wash up, social distance)

 My GFR (the numbers above the arc in the photo to the left and defined later in this blog) is usually between 49% and 59%. That means at any given time I’m missing quite a bit of the function normal kidneys would have. In other words, my kidneys are working more than twice as hard as those of someone without kidney disease. This is a fact that’s easy to forget now that I have the renal diet down pat … until I get sick… and it takes me longer to recuperate… or I slide right into another illness.
My GFR (the numbers above the arc in the photo to the left and defined later in this blog) is usually between 49% and 59%. That means at any given time I’m missing quite a bit of the function normal kidneys would have. In other words, my kidneys are working more than twice as hard as those of someone without kidney disease. This is a fact that’s easy to forget now that I have the renal diet down pat … until I get sick… and it takes me longer to recuperate… or I slide right into another illness.