Last week, I mentioned that my renal/diabetes dietician had suggested Magic Spoon cereal since it’s low carbohydrate. I didn’t care for it. Marc Hernandez of Uhling Consulting was surprised, since he and his family really liked it. We tried to figure out why I didn’t. Then Marc hit on something. Maybe I was a super taster. Oh goody, a new concept for me.

Let’s get a definition for super taster before we go any further. According to Healthline, a super taster is
“… a person who tastes certain flavors and foods more strongly than other people.”
Well, that’s obvious. We need more. And that’s what I discovered on LiveScience:
“… The tally of little mushroom-shaped projections on the tongue, called fungiform papillae, reveals a person’s tasting prowess or deficit.
Nestled within the walls of these tiny bumps are our taste receptors, called taste buds, which register the five currently recognized tastes: bitterness, saltiness, sourness, sweetness and umami (savoriness). Touch receptors in the fungiform papillae also help us ‘feel’ our food’s texture and temperature.
The application of blue food coloring makes the papillae easier to count. In a 6-millimeter diameter circle, which is ‘about the size of a hole punch,’ Bartoshuk said, supertasters can have as many as 60 fungiform papillae packed into the small space; nontasters can have as few as five.”
Wait, there’s more information from the discoverer and coiner of the term super tasters from CBC Radio:
“In Bartoshuk’s research, she found that 25 per cent of people are incredibly sensitive to a bitter tasting chemical known as 6-n-propylthiouracil, or PROP. Another 25 per cent, deemed non-tasters, can’t detect PROP at all, she says, while the remaining 50 per cent are considered average tasters.

While affixing super to anything sounds great, being a supertaster can actually be quite difficult, says Bartoshuk, who coined the terms supertaster and non-taster.
Supertasters are differentially more sensitive to bitter. Having more tastebuds means there are also more pain receptors, and that’s why supertasters often can’t handle spicy foods and generally avoid anything bitter. As a result, they are often seen as picky eaters.
However, their aversion to bitterness is evolutionary, says Bartoshuk.
‘Supertasters are differentially more sensitive to bitter’ than the average person.
Bartoshuk says there are 25 different bitter genes expressing 25 different bitter receptors.
‘Why would nature do that? Because bitter is our poison detection system.’”
So, do I feel honored or cursed to possibly be a super taster? I think I need more information.
Wow! While more testing is needed, I found this article on National Geographic encouraging:
“Henry Barham, a rhinologist at the Baton Rouge General Medical Center, in Louisiana, published a study in the medical journal JAMA Network Open on May 25 that analyzed nearly 2,000 patients and found that ‘supertasters’—individuals who are overly sensitive to some bitter compounds—were less likely to test positive for the virus. If this association holds true, it implies, for example, that people who don’t find broccoli too bitter are in a higher risk group for severe COVID-19.
‘This is a very interesting study that suggests that receptors on our tongue that allow us to sense bitter flavors are also linked to our vulnerability to respiratory infections like COVID-19,’ says David Aronoff, director of the division of infectious diseases at Vanderbilt University Medical Center, in Nashville, Tennessee, who was not involved with this research. That taste receptors may also be involved with immunity is surprising, he says….

According to Aronoff, the study has limitations. The relatively small number of adults examined were in a fairly narrow age range, so it’s not known whether the correlation between taste preferences and COVID-19 severity exists in children or the elderly. In addition, he says, the population studied may differ in unknown ways that influenced the results.”
Hmmm, and that has to do with the renal diet or diabetes how? Back to Healthline for the answer:
“Pros of being a supertaster:
May weigh less than average or non-tasters. That’s because supertasters often avoid sugary, fatty foods that are often packed with calories. These flavors can be too overwhelming and unenjoyable, just like bitter flavors.
Are less likely to drink and smoke. The bittersweet flavors of beer and alcohol are often too bitter for supertasters. Plus, the flavor of smoke and tobacco can be too harsh, too.
Cons of being a supertaster
Eat few healthy vegetables. Cruciferous vegetables, including Brussels sprouts, broccoli, and cauliflower, are very healthy. Supertasters often avoid them, however, because of their bitter flavors. This can lead to vitamin deficiencies.
May be at a higher risk for colon cancer. The cruciferous vegetables they can’t tolerate are important for digestive health and helping lower the risk of certain cancers. People who don’t eat them may have more colon polyps and higher cancer risks.
May have an increased risk for heart disease. Salt masks bitter flavors, so supertasters tend to use it on many foods. Too much salt, however, can cause health problems, including high blood pressure and heart disease.
May be picky eaters. Foods that are too bitter just aren’t pleasant. That limits the number of foods many supertasters will eat.”
Here are some reminders to help you see the connections.
Pros:
Obesity can lead to diabetes. Smoking and drinking can hasten your CKD.
Cons:
SALT! The bane of CKD. Also, being picky means you may not be fulfilling your nutritional needs and, instead filling up on foods that will only worsen your CKD and/or diabetes.
After all this researching, I’ve come to the conclusion that I am not among the 25% of the population that are super tasters. Nor am I part of the 25% of non-tasters. Yep, I’m part of the 50% of average tasters. I just happen not to care for the taste of Magic Spoon. Again, that doesn’t mean you won’t. After all, Marc and his family like it.
Until next week,
Keep living your life!


























































































 No, that’s not the result of misplacing my fingers on the keyboard. According to
No, that’s not the result of misplacing my fingers on the keyboard. According to 


 Get ready for this: those with Chronic Kidney Disease have a 12.8% higher incidence of abdominal incisional hernia according to a PubMed 2013 study published on ResearchGate’s site available at
Get ready for this: those with Chronic Kidney Disease have a 12.8% higher incidence of abdominal incisional hernia according to a PubMed 2013 study published on ResearchGate’s site available at 
 tissues, which can cause swelling and pain in the surrounding area.
tissues, which can cause swelling and pain in the surrounding area. I’ll explain that in a minute, but first – on this Labor Day weekend – I want to thank all the readers who have liked individual blogs. These likes let me know I’m writing about topics that interest you.
I’ll explain that in a minute, but first – on this Labor Day weekend – I want to thank all the readers who have liked individual blogs. These likes let me know I’m writing about topics that interest you.
 There are some very common drugs on this list. As Chronic Kidney Disease patients, we are warned away from NSAIDS. I’ve been warned about Ciprofloxacin, too, and PPIs, but diuretics? Most of the other drugs we’d have to ask our doctors about when and if they’re prescribed. Then again, I ask my family doctor to check the effect of the drug on the kidneys when she prescribes a drug. She happily does so.
There are some very common drugs on this list. As Chronic Kidney Disease patients, we are warned away from NSAIDS. I’ve been warned about Ciprofloxacin, too, and PPIs, but diuretics? Most of the other drugs we’d have to ask our doctors about when and if they’re prescribed. Then again, I ask my family doctor to check the effect of the drug on the kidneys when she prescribes a drug. She happily does so. his army across the
his army across the  A computerized tomography (CT) scan combines a series of X-ray images taken from different angles around your body and uses computer processing to create cross-sectional images (slices) of the bones, blood vessels and soft tissues inside your body. CT scan images provide more-detailed information than plain X-rays do.”
A computerized tomography (CT) scan combines a series of X-ray images taken from different angles around your body and uses computer processing to create cross-sectional images (slices) of the bones, blood vessels and soft tissues inside your body. CT scan images provide more-detailed information than plain X-rays do.” Of course, now we need to know why we shouldn’t be having this contrast material. Radiology Affiliates Imagining at
Of course, now we need to know why we shouldn’t be having this contrast material. Radiology Affiliates Imagining at 
 “Your immune system is a complex network of cells, tissues, and organs that work together to defend against germs. It helps your body to recognize these ‘foreign’ invaders. Then its job is to keep them out, or if it can’t, to find and destroy them.”
“Your immune system is a complex network of cells, tissues, and organs that work together to defend against germs. It helps your body to recognize these ‘foreign’ invaders. Then its job is to keep them out, or if it can’t, to find and destroy them.”
 Why not, you may be asking yourself. Easy answer? I’m allergic to them. Wait just a minute here. What exactly does allergic mean and how will this affect your Chronic Kidney Disease?
Why not, you may be asking yourself. Easy answer? I’m allergic to them. Wait just a minute here. What exactly does allergic mean and how will this affect your Chronic Kidney Disease?
 I’ve satisfied myself that, just as with my food allergies, my sensitivity to lactose, wheat, fructose syrup, and acidic foods will not harm my kidneys. Although, they may cause me to read more food labels than I usually do. Hopefully, you’re satisfied that your food allergies and sensitivities will not harm your kidneys. If you’re still concerned, speak with your nephrologist or renal dietitian.
I’ve satisfied myself that, just as with my food allergies, my sensitivity to lactose, wheat, fructose syrup, and acidic foods will not harm my kidneys. Although, they may cause me to read more food labels than I usually do. Hopefully, you’re satisfied that your food allergies and sensitivities will not harm your kidneys. If you’re still concerned, speak with your nephrologist or renal dietitian.

 “A vascular access is a hemodialysis patient’s lifeline, because it makes life-saving hemodialysis treatments possible. Hemodialysis is a treatment for kidney failure that uses a machine to send the patient’s blood through a filter, called a dialyzer, outside the body. The access is a surgically created vein used to remove and return blood during hemodialysis. The blood goes through a needle, a few ounces at a time. The blood then travels through a tube that takes it to the dialyzer. Inside the dialyzer, the blood flows through thin fibers that filter out wastes and extra fluid. The machine returns the filtered blood to the body through a different tube. A vascular access lets large amounts of blood flow continuously during hemodialysis treatments to filter as much blood as possible per treatment. About a pint of blood flows through the machine every minute. A vascular access should be in place weeks or months before the first hemodialysis treatment.”
“A vascular access is a hemodialysis patient’s lifeline, because it makes life-saving hemodialysis treatments possible. Hemodialysis is a treatment for kidney failure that uses a machine to send the patient’s blood through a filter, called a dialyzer, outside the body. The access is a surgically created vein used to remove and return blood during hemodialysis. The blood goes through a needle, a few ounces at a time. The blood then travels through a tube that takes it to the dialyzer. Inside the dialyzer, the blood flows through thin fibers that filter out wastes and extra fluid. The machine returns the filtered blood to the body through a different tube. A vascular access lets large amounts of blood flow continuously during hemodialysis treatments to filter as much blood as possible per treatment. About a pint of blood flows through the machine every minute. A vascular access should be in place weeks or months before the first hemodialysis treatment.”
 Here’s hoping those of you in the U.S.A. had a safe and thoughtful July 4th. This is a peculiar year with different kinds of celebration or none at all.
Here’s hoping those of you in the U.S.A. had a safe and thoughtful July 4th. This is a peculiar year with different kinds of celebration or none at all.

 “What is nephrogenic diabetes insipidus?
“What is nephrogenic diabetes insipidus?

 It seems that most of them are taking lithium to help control the bipolar disorder. Okay, I’ll bite: what is lithium? Drugs.com at
It seems that most of them are taking lithium to help control the bipolar disorder. Okay, I’ll bite: what is lithium? Drugs.com at 
 The most common problem from taking lithium is a form of diabetes due to kidney damage called nephrogenic diabetes insipidus. This type of diabetes is different than diabetes mellitus caused by high blood sugar. In nephrogenic diabetes insipidus, the kidneys cannot respond to anti-diuretic hormone (ADH), a chemical messenger that controls fluid balance. This results in greater than normal urine out-put and excessive thirst. It can be hard to treat nephrogenic diabetes insipidus.”
The most common problem from taking lithium is a form of diabetes due to kidney damage called nephrogenic diabetes insipidus. This type of diabetes is different than diabetes mellitus caused by high blood sugar. In nephrogenic diabetes insipidus, the kidneys cannot respond to anti-diuretic hormone (ADH), a chemical messenger that controls fluid balance. This results in greater than normal urine out-put and excessive thirst. It can be hard to treat nephrogenic diabetes insipidus.” Responsum for CKD does just that, but I’ll let them explain their app themselves. This is from their April 28th blog at
Responsum for CKD does just that, but I’ll let them explain their app themselves. This is from their April 28th blog at  About Responsum Health
About Responsum Health “the use of ultrasound to examine the structure and functioning of the heart for abnormalities and disease”
“the use of ultrasound to examine the structure and functioning of the heart for abnormalities and disease”
 A technician (sonographer) spreads gel on a device (transducer).
A technician (sonographer) spreads gel on a device (transducer).
 Now the biggie: What causes neuropathy? MedicineNet at
Now the biggie: What causes neuropathy? MedicineNet at 
 Time for another reader question, but first, let’s pay attention to what day today is. Many people see today as the day for bar-b-ques or backyard ball games (or, at least, they did before Covid 19). When I married Bear a little more than seven years ago, he explained about Memorial Day. I knew it was to honor those who died protecting us, but it was so much more meaningful when explained by a veteran… someone who didn’t die protecting us and lived on to meet me and marry me. So give some quiet thoughts to these men and woman today, will you?
Time for another reader question, but first, let’s pay attention to what day today is. Many people see today as the day for bar-b-ques or backyard ball games (or, at least, they did before Covid 19). When I married Bear a little more than seven years ago, he explained about Memorial Day. I knew it was to honor those who died protecting us, but it was so much more meaningful when explained by a veteran… someone who didn’t die protecting us and lived on to meet me and marry me. So give some quiet thoughts to these men and woman today, will you? apparent that the disease is improving, doctors slowly reduce the corticosteroid dose and eventually hope to discontinue it completely. When cyclophosphamide is used, it is only given until the time of remission (usually around 3 to 6 months), after which time it is switched to another immunosuppressive agent, such as methotrexate, azathioprine (Imuran®), or mycophenolate mofetil (Cellcept®) to maintain remission. The treatment duration of the maintenance immunosuppressive medication may vary between individuals. In most instances, it is given for a minimum of 2 years before consideration is given to slowly reduce the dose toward discontinuation.”
apparent that the disease is improving, doctors slowly reduce the corticosteroid dose and eventually hope to discontinue it completely. When cyclophosphamide is used, it is only given until the time of remission (usually around 3 to 6 months), after which time it is switched to another immunosuppressive agent, such as methotrexate, azathioprine (Imuran®), or mycophenolate mofetil (Cellcept®) to maintain remission. The treatment duration of the maintenance immunosuppressive medication may vary between individuals. In most instances, it is given for a minimum of 2 years before consideration is given to slowly reduce the dose toward discontinuation.” symptoms of the disease and treating the underlying autoimmune activity. It may include use of steroids [Gail here: Remember they’re used in treating this reader’s other disease, too.] and other anti-inflammatory agents,
symptoms of the disease and treating the underlying autoimmune activity. It may include use of steroids [Gail here: Remember they’re used in treating this reader’s other disease, too.] and other anti-inflammatory agents,  I can just see your faces now. Huh? What is that? The concept makes sense, but the word doesn’t. Do you remember my mentioning that one of the joys of being a writer is that you make up words? Well, that’s one I made up right after my doctor talked with me about vitamin D and immunity. He was talking about warding off a reoccurrence of cancer, but when I started researching I found that it has to do with all immunity.
I can just see your faces now. Huh? What is that? The concept makes sense, but the word doesn’t. Do you remember my mentioning that one of the joys of being a writer is that you make up words? Well, that’s one I made up right after my doctor talked with me about vitamin D and immunity. He was talking about warding off a reoccurrence of cancer, but when I started researching I found that it has to do with all immunity.
 Vitamin D is known to enhance the function of immune cells, including T-cells and macrophages, that protect your body against pathogens….
Vitamin D is known to enhance the function of immune cells, including T-cells and macrophages, that protect your body against pathogens….


 Do Not Smoke
Do Not Smoke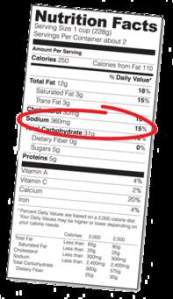
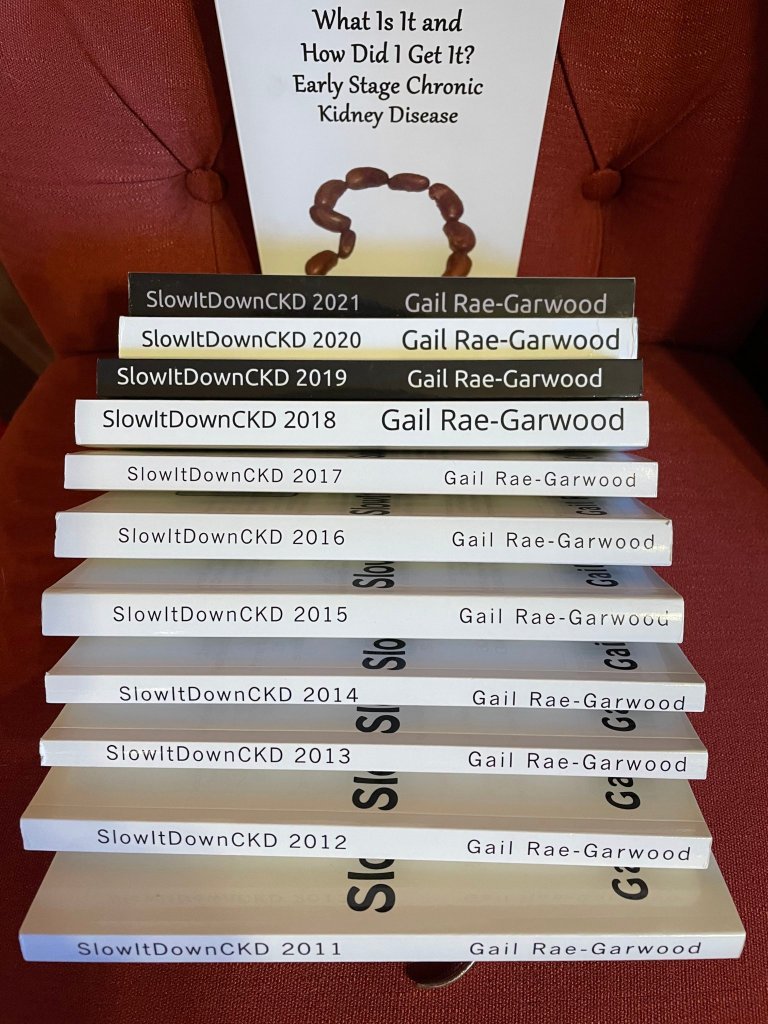
 awareness to those living with (and without) Chronic Kidney Disease.
awareness to those living with (and without) Chronic Kidney Disease. One such person is Steve L. Belcher. After I realized I’ve been seeing his name again and again on Facebook, I decided to ask him to guest blog. I certainly learned a lot from his blog and I hope you do, too. This is not a competition among Chronic Kidney Disease awareness advocates, but an informal coalition. We all want you to know as much as you can about this disease we share. Steve’s blog explains the background for all the shows he broadcasts. Kudos, my friend, kudos.
One such person is Steve L. Belcher. After I realized I’ve been seeing his name again and again on Facebook, I decided to ask him to guest blog. I certainly learned a lot from his blog and I hope you do, too. This is not a competition among Chronic Kidney Disease awareness advocates, but an informal coalition. We all want you to know as much as you can about this disease we share. Steve’s blog explains the background for all the shows he broadcasts. Kudos, my friend, kudos. President of Operations. During our early beginnings, we began broadcasting Urban Renal Talk with Tamika and Steve from our cellphones to our Facebook Page. The Urban Renal Talk with Tamika and Steve broadcast was created to interview kidney patients and professionals making a difference in the chronic kidney disease community. Since the beginning Urban Renal Talk with Tamika and Steve has come a long way with over four hundred broadcast shows to date. Our shows consist of digital broadcasting, which is the distribution of audio or video content to a dispersed audience via any electronic mass communication medium.
President of Operations. During our early beginnings, we began broadcasting Urban Renal Talk with Tamika and Steve from our cellphones to our Facebook Page. The Urban Renal Talk with Tamika and Steve broadcast was created to interview kidney patients and professionals making a difference in the chronic kidney disease community. Since the beginning Urban Renal Talk with Tamika and Steve has come a long way with over four hundred broadcast shows to date. Our shows consist of digital broadcasting, which is the distribution of audio or video content to a dispersed audience via any electronic mass communication medium.

 that this was all we had in the way of protecting ourselves (as much as possible) from contacting the virus here in the United States. The precautions weren’t that much different than the precautions for everyone else.
that this was all we had in the way of protecting ourselves (as much as possible) from contacting the virus here in the United States. The precautions weren’t that much different than the precautions for everyone else.
 This is still paltry information at best. Emedicine at
This is still paltry information at best. Emedicine at 
 https://www.prevention.com/health/a31245792/coronavirus-high-risk-groups/
https://www.prevention.com/health/a31245792/coronavirus-high-risk-groups/ husband, who doesn’t have CKD, loved them, too. I enjoyed their pasta products, too. Now, lest you get the wrong idea, I am not endorsing this company because I don’t know what others like it are available. However, I wanted to know about their products… which may very well be similar to the products of other such companies and, therefore, helpful to CKD patients.
husband, who doesn’t have CKD, loved them, too. I enjoyed their pasta products, too. Now, lest you get the wrong idea, I am not endorsing this company because I don’t know what others like it are available. However, I wanted to know about their products… which may very well be similar to the products of other such companies and, therefore, helpful to CKD patients.
 from
from 


