It amazes me that after writing this blog for over a dozen years, I can still happen across something about the kidneys that I didn’t know. This week it’s Acute Tubular Necrosis. Have you ever heard of this before?
Way back in 2010, I defined acute in What Is It and How Did I Get It? Early Stage Kidney Disease:

“Acute: Extremely painful, severe, or serious, quick onset, of short duration; the opposite of chronic.”
I’m going to go back even further back to my college textbook, Latin & Greek in Current Use, Second Edition, for the definition of necrosis:
“corpse”
Or, updated for our purposes, dead.
I think we can handle tubular with my favorite dictionary, the Merriam-Webster Dictionary:
“having the form of or consisting of a tube. made or provided with tubes.”
Putting it all together, it’s the sudden onset of dead tubes. It can’t be that simplistic and this definition doesn’t make that much sense. So, I went to Medline for a more comprehensive definition:
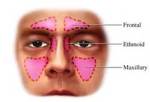
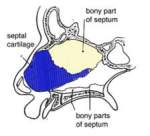
“Acute tubular necrosis (ATN) is a kidney disorder involving damage to the tubule cells of the kidneys, which can lead to acute kidney failure. The tubules are tiny ducts in the kidneys that help filter the blood when it passes through the kidneys.
Got it. Well, what can cause ATN? The Cleveland Clinic was helpful here:
“The most frequent causes of acute tubular necrosis are a stroke or a heart attack, conditions that reduce oxygen to the kidneys.
Chemicals can also damage the tubules. These include X-ray contrast dye, anesthesia drugs, antibiotics and other toxic chemicals.”
That’s one of the reasons cardiology and nephrology are so connected. Avoid cardiology problems and you’re helping yourself to avoid ATN. One of the three kinds of stroke is hemorrhagic. It’s caused by a burst or blockage of blood vessels in your brain and can be affected by any blood vessel problem. One of the causes of hemorrhagic stroke is high blood pressure which just happens to be one of the causes of chronic kidney disease. It’s also logical; if your blood can’t reach your kidneys due to the blockage, your kidneys will be damaged.
Well, how do you know if you have ATN? Healthline lists the symptoms for us:
“The symptoms of ATN vary depending on its severity. You may:

feel drowsy even during the day
feel lethargic or physically drained
be excessively thirsty or experience dehydration
urinate very little or not at all
retain fluid or experience swelling in your body
have episodes of confusion
experience nausea or vomiting”
I’m glad I stumbled across ATN. It sounds like something important all CKD patients should know about. By the way, do you see a cardiologist? Speak with your nephrologist to see if it’s something they’d recommend.
We know what ATN is, what causes it, and what the symptoms are now, but what do you do about it if you find you have ATN?
Wait. I have to share this with you. It’s Medscape’s information about ATN that we haven’t come across yet:
“Acute tubular necrosis (ATN) is the most common cause of acute kidney injury (AKI) in the renal category (that is, AKI in which the pathology lies within the kidney itself). The term ATN is actually a misnomer, as there is minimal cell necrosis and the damage is not limited to tubules.”
That sounds worse! We’d better get on to what to do about ATN if you find you have it. WebMD had quite a bit of information about treatment:

“The exact treatment that your doctor recommends will depend on the cause of your acute tubular necrosis.
If your acute tubular necrosis is caused by some form of poisoning, the most important treatment will be clearing the harmful substance out of your body. Then, you need to make sure that you know how the poison got into your body so it doesn’t happen again.
Normally, your kidneys will be able to heal on their own. This means that your treatment will be focused on preventing the buildup of fluids and waste products in your body.
Your treatment phase can last anywhere from a few days to over six weeks. It depends on how badly damaged your kidneys are. Treatment methods can include:
Dialysis. In some cases, your doctor may decide that you need dialysis, a process that removes waste, salt, and fluids to prevent them from building up in the body while your kidneys are healing. They’ll decide this on a case-by-case basis.
Dietary changes. Sometimes, you’ll also need to change your diet during your recovery. Helpful changes could include limiting how much fluid and sodium you eat and drink. This way, you don’t add to the fluid build-up that’s caused by the acute tubular necrosis.
Medications. In some cases, your doctor will prescribe medications to take during your recovery. These include ones to help increase how often you urinate or to control potassium levels in your body.
If this condition is left untreated, your kidneys could fail. This could mean that you need to make life-long changes to manage the symptoms from the tissue damage.”
The Merck Manual (Consumer Version) offers us both good and bad news:
“Outcome depends on correction of the disorder that caused acute tubular necrosis. If that disorder responds rapidly to treatment, kidney function usually returns to normal in 1 to 3 weeks. Prognosis is usually better if people’s urine volume exceeds 400 mL (about 13.5 ounces) every 24 hours. People who are more seriously ill, especially those who require care in an intensive care unit, have a higher risk of death.”

There’s another reason to take extra good care of both your heart and your kidney health. Should you end up with ATN, you want to be one of those “otherwise healthy patients.” It all sounds bad but be careful rather than afraid.
Until next week,
Keep living your life!




 We all know diabetes raises your risk of developing Chronic Kidney Disease. But why? What’s the mechanism behind the fact? As far as I’m concerned, it’s time to find out.
We all know diabetes raises your risk of developing Chronic Kidney Disease. But why? What’s the mechanism behind the fact? As far as I’m concerned, it’s time to find out.
 good idea to limit red meat, and avoid processed meats.
good idea to limit red meat, and avoid processed meats.
 Happy New Year! Here’s wishing you all a very healthy one. I, on the other hand, found myself in the cardiologist’s office the very first week of 2019. That was odd for me.
Happy New Year! Here’s wishing you all a very healthy one. I, on the other hand, found myself in the cardiologist’s office the very first week of 2019. That was odd for me.
 Notice I capitalized may. That’s because, in my case, there apparently was no blockage. My cardiologist had a different view of things. He felt there wasn’t a problem unless the difference in readings between your two arms is more than 20 points and that your blood pressure would have to be much higher than my slightly elevated blood pressure before this could be considered a problem.
Notice I capitalized may. That’s because, in my case, there apparently was no blockage. My cardiologist had a different view of things. He felt there wasn’t a problem unless the difference in readings between your two arms is more than 20 points and that your blood pressure would have to be much higher than my slightly elevated blood pressure before this could be considered a problem.
 When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
 Better Information
Better Information































![Rae%208x10%205792%20Sepia%20TinType[1]](https://gailraegarwood.wordpress.com/wp-content/uploads/2011/03/rae208x1020579220sepia20tintype1.jpg?w=120)





















