Hello, hello, and a belated welcome to National Kidney Month. This year, for a change, I decided to go to a non-medical site for a clear explanation of what this month is. The entire blog [except my introduction, of course.] is from National Today, a site committed to which celebrations are on which day[s]:
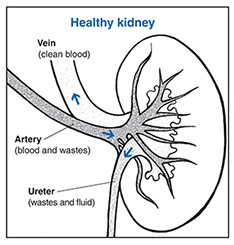
“March is dedicated to National Kidney Month. The kidneys, two bean-shaped organs located in the back of the abdomen, perform crucial functions to filter out toxins, produce red blood cells, and regulate pH. They filter about half a cup of blood every hour, creating urine from harmful and unnecessary waste.
When kidneys fail to function properly, waste builds up in the blood and leads to a weakened system and a host of problems like anemia, nerve damage, and high blood pressure. Chronic kidney disease(CKD) affects more than 1 in 7 American adults and is the 9th leading cause of death in the U.S.
HISTORY OF NATIONAL KIDNEY MONTH
National Kidney Month, observed every March, brings awareness to kidney health and encourages people to support kidney disease research and take steps to keep their own kidneys safe and healthy.
Kidneys filter blood, make urine, and produce the red blood cells that carry oxygen through your body. These vital organs also control blood pressure and produce vitamin D to keep bones strong.
Malfunctioning kidneys can lead to painful kidney stones and infections that, left untreated, require a transplant. Some pre-existing conditions, like high blood pressure and diabetes, put you at increased risk for kidney disease.
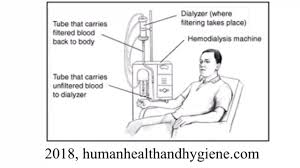
Chronic Kidney Disease(CKD) affects almost 40 million American adults. In 2016, three-quarters of a million people in the U.S. required dialysis or a kidney transplant. Dialysis and kidney transplants, the only treatment options for severe kidney failure, are difficult, expensive, and not always available. Patients seeking new organs may not always get them in time to survive; in the U.S., twelve people die each day waiting for a kidney.
To prevent kidney disease, the National Kidney Foundation recommends taking proactive steps to keep your kidneys healthy and prevent the onset of CKD. You can protect your kidneys by managing high blood pressure, making healthy food and drink choices, and reducing stress.
The National Kidney Foundation grew out of a mother’s determination to further research into treatment for kidney conditions. When her infant son was diagnosed with nephrosis, Ada DeBold started the Committee for Nephrosis Research to organize efforts to find treatments and connect patients and doctors. DeBold continued crusading for the organization, which eventually became the National Kidney Foundation. The Foundation conducts fundraising to support important research into the treatment and prevention of kidney disease.
NATIONAL KIDNEY MONTH TIMELINE
1984
National Organ Transplant Act Passes
The NOTA establishes the National Organ Procurement and Transplantation Network, which maintains an organ matching registry to address organ shortages and streamline the donation process.
1954
First Successful Kidney Transplant
The first successful kidney transplant is performed between two identical twins in Boston.
1943
Dialysis Invented
Dutch doctor Willem Kolff invents the ‘artificial kidney’ to clean the blood of kidney failure patients.
1902
Animal Experiments
The first successful kidney transplants in animals are performed at the Vienna Medical School.
NATIONAL KIDNEY MONTH FAQS
What month is National Kidney Month?
National Kidney Month is observed annually during the month of March.
Is there a ribbon for kidney disease?
Kidney Disease Awareness is symbolized by the color green. Purchase green ribbons, green wristbands, or green magnets directly from a Kidney Disease Awareness non profit in order to help raise funds for treatments.

What are the symptoms of chronic kidney disease?
Symptoms include difficulty urinating or less urine, sweeping in the extremities, shortness of breath, nausea, and feeling cold and tired. If you experience chronic symptoms that you suspect are related to kidney function, consult your physician.
HOW TO OBSERVE NATIONAL KIDNEY MONTH
- Join the organ donor registry
Most organ donations come from deceased people. Register to be an organ donor when you die and your healthy organs and tissue can save dozens of lives.
- Donate to a kidney non-profit
Non-profit organizations do the important work of raising awareness about kidney disease, providing resources and assistance to patients, and connecting patients, doctors, and donors.
- Be good to your kidneys
Are you keeping your kidneys healthy? Aim for a lower intake of sodium and sugars, more whole grains and low-fat dairy, and regular exercise to reduce your risk of kidney disease, high blood pressure, diabetes, and other diseases.
5 FASCINATING FACTS ABOUT KIDNEYS
- You only need one kidney to live
Although you’re born with two kidneys, each of which have about 1.5 million blood-filtering units(nephrons), you only need about 300,000 nephrons to filter your blood properly.
- Your kidneys are lopsided
The right kidney is slightly smaller and sits lower than the left to make room for another important organ, the liver.
- You can drink too much water
This can cause a condition called hyponatremia, which, though not common, can damage the kidneys.
- Sausage casing and orange juice cans
Willem Kolff, who invented the first artificial kidney that led to today’s dialysis technology, used sausage casings, orange juice cans, and a washing machine to create a rudimentary blood cleaning mechanism.
- Climate change may increase kidney disease
As parts of the world get warmer, the dehydration that leads to kidney disease is likely to rise among manual laborers.
WHY NATIONAL KIDNEY MONTH IS IMPORTANT
- It reminds us to be good to our bodies
Make sure you take care of your body and your vital internal organs so they can continue taking care of you.
- It’s a chance to express gratitude for our health
If you have fully functional kidneys, be grateful! Take a minute to feel gratitude for all the internal organs that do the invisible, daily work of keeping us alive.
- It shows that science is awesome
Just a few decades ago, kidney disease could mean a death sentence. Today, although it’s still a serious and frightening illness, we can often fight off kidney failure with dialysis and organ transplants.”
Many thanks to National Today for their simple, straight forward explanation of National Kidney Month.
Until next week,
Keep living your life!