I have been so stressed lately. It’s the usual: Covid-19, the elections, etc. But then there are the personal reasons: my upcoming surgery, Bear’s cataract surgery and being his caretaker, the third under-the-slab water leak in our house, and my brother’s ill health come to mind right away. I do take time to quietly read, play Word Crush, or watch a movie, but the stress is still there… and my blood glucose numbers are going up. “Is there a correlation?” I wondered.
You may remember (I certainly do) that Healthline included this blog in the Best Kidney Disease Blogs for 2016 & 2017. They like my work; I like theirs, so I went to their website to see what I could find about stress and diabetes. I have diabetes type 2, by the way. That’s the type in which you produce insulin, but your body doesn’t use it well.

Okay, now let’s see what Healthline at https://bit.ly/2TIHwWZ has to say:
“… But there’s a problem. The body can’t differentiate between danger and stress. Both trigger fight-or-flight.
So today’s most common ‘danger’ isn’t wild animals. It’s the letter from the IRS. There’s no quick resolution — no violent fight, no urgent need to run for miles. Instead, we sit in our sedentary homes and workplaces, our bodies surging with sugar, with no way to burn it off.
That’s how stress messes with diabetes. Acute stress floods us with unwanted (and un-medicated) sugar. Chronic stress is like a leaking faucet, constantly dripping extra sugar into our systems. The impact on blood sugar caused by stress is so significant that some researchers feel it serves as a trigger for diabetes in people already predisposed to developing it.”
Wait a minute here. “Acute stress floods us with unwanted (and un-medicated) sugar.” How does it do that? The answer I liked best is from Lark at https://bit.ly/3ebZU4b. Yes, Lark is a company that produces electronic aids for various stages of diabetes, but it also offers short, easy to understand explanations of what’s happening to your diabetes during different situations.
“Cortisol signals your brain and body that it is time to prepare to take action. You may be able feel this as your heart pounds and muscles tense. At the same time, what you may not feel is that cortisol signals a hormone called glucagon to trigger the liver to release glucose (sugar) into your bloodstream. The result: higher blood sugar.
Cortisol’s role in preparing your body for action goes beyond mobilizing glucose stores. Cortisol also works to make sure that the energy that you might spend (whether fighting a bear or running to stop your toddler from toddling into the street) gets replenished. That means you may feel hungry even when you do not truly need the food – and that can lead to weight gain. Again, the result is an increase in blood sugar.”

Quick reminder:
“Think of cortisol as nature’s built-in alarm system. It’s your body’s main stress hormone. It works with certain parts of your brain to control your mood, motivation, and fear.
Your adrenal glands — triangle-shaped organs at the top of your kidneys — make cortisol.
It’s best known for helping fuel your body’s ‘fight-or-flight’ instinct in a crisis, but cortisol plays an important role in a number of things your body does. For example, it:
- Manages how your body uses carbohydrates, fats, and proteins
- Keeps inflammation down
- Regulates your blood pressure
- Increases your blood sugar (glucose)
- Controls your sleep/wake cycle
- Boosts energy so you can handle stress and restores balance afterward”
Thank you to WebMD at https://wb.md/35RaDgr for the above information.
Let’s get back to how we end up with excess sugar in our blood due to both acute (sudden) and/or chronic (long term) stress. Diabetes Education Online, part of the Diabetes Teaching Center at the University of California, San Francisco, offers the following explanation. You can find out more by going to their website at https://bit.ly/3oNXgqi.
“During stressful situations, epinephrine (adrenaline), glucagon, growth hormone and cortisol play a role in blood sugar levels. Stressful situations include infections, serious illness or significant emotion stress.
When stressed, the body prepares itself by ensuring that enough sugar or energy is readily available. Insulin levels fall, glucagon and epinephrine (adrenaline) levels rise and more glucose is released from the liver. At the same time, growth hormone and cortisol levels rise, which causes body tissues (muscle and fat) to be less sensitive to insulin. As a result, more glucose is available in the blood stream.”

Now I’m stressed about being stressed… and that’s after trying to keep my stress levels down so I don’t make my Chronic Kidney Disease worse… now I find it’s also making my diabetes worse. What, in heaven’s name, will happen if I continue to be this stressed?
I went right to The National Kidney Foundation at https://bit.ly/2HQVsvs for an answer I could trust.
“The combined impacts of increased blood pressure, faster heart rate, and higher fats and sugar in your blood can contribute to a number of health problems, including high blood pressure, diabetes, and heart disease (also known as cardiovascular disease).
Stress and uncontrolled reactions to stress can also lead to kidney damage. As the blood filtering units of your body, your kidneys are prone to problems with blood circulation and blood vessels. High blood pressure and high blood sugar can place an additional strain or burden on your kidneys. People with high blood pressure and diabetes are at a higher risk for kidney disease. People with kidney disease are at higher risk for heart and blood vessel disease. If you already have heart and blood vessel disease and kidney disease, then the body’s reactions to stress can become more and more dangerous.”
Oh, my! I think I’d better quietly read, play Word Crush, or watch a movie right now.

Before I leave, I did want to let you know a $10 million Kidney Prize competition has been launched. If you’re seriously interested, go to https://akp.kidneyx.org. According to their website, KidneyX is
“The Kidney Innovation Accelerator (KidneyX), a public-private partnership between the U.S. Department of Health and Human Services (HHS) and the American Society of Nephrology (ASN), is accelerating innovation in the prevention, diagnosis, and treatment of kidney diseases.”
Until next week,
Keep living your life!





 lancet, the less the poke to get that one drop of blood needed for testing hurts.
lancet, the less the poke to get that one drop of blood needed for testing hurts.
 “the use of ultrasound to examine the structure and functioning of the heart for abnormalities and disease”
“the use of ultrasound to examine the structure and functioning of the heart for abnormalities and disease”


 Do Not Smoke
Do Not Smoke

 to me, my writing mentor and friend… and I miss her terribly. Thinking about Audre led me to thinking about my younger daughter (Abby) who won the Black History Month Essay Contest in her elementary school several years in a row by writing about Audre’s and my friendship.
to me, my writing mentor and friend… and I miss her terribly. Thinking about Audre led me to thinking about my younger daughter (Abby) who won the Black History Month Essay Contest in her elementary school several years in a row by writing about Audre’s and my friendship. Kountz:
Kountz: should be noted in Black History Month in the future since the general public needs to be aware of Chronic Kidney Disease in order to be tested and, ultimately, treated. Dr. Bignall echoes my own thoughts.
should be noted in Black History Month in the future since the general public needs to be aware of Chronic Kidney Disease in order to be tested and, ultimately, treated. Dr. Bignall echoes my own thoughts. I felt compelled to include Dr. Charles DeWitt Watts who, while not a nephrologist, was eminent in breaking racial barriers so we could have Black nephrologists available to us. The following is from Duke University Medical Center and Library at
I felt compelled to include Dr. Charles DeWitt Watts who, while not a nephrologist, was eminent in breaking racial barriers so we could have Black nephrologists available to us. The following is from Duke University Medical Center and Library at  given my work and experience on this topic.
given my work and experience on this topic. ”Please help. I just got blood results back from my yearly physical and saw that my eGFR was 55 and my creatinine was 1.09. After speaking to my GP she told me my results were nothing to ‘be concerned about’. Since the 2 above mentioned results were highlighted in red I figured perhaps I should ‘concern’ myself about it and research what it could possibly mean. I was shocked to read that it indicated kidney disease. When I told my doctor of my findings, she again pushed it off as nothing to worry about. Am I over reacting? Thanks for any help you can give me.”
”Please help. I just got blood results back from my yearly physical and saw that my eGFR was 55 and my creatinine was 1.09. After speaking to my GP she told me my results were nothing to ‘be concerned about’. Since the 2 above mentioned results were highlighted in red I figured perhaps I should ‘concern’ myself about it and research what it could possibly mean. I was shocked to read that it indicated kidney disease. When I told my doctor of my findings, she again pushed it off as nothing to worry about. Am I over reacting? Thanks for any help you can give me.” “… a loop diuretic (water pill) that prevents your body from absorbing too much salt, allowing the salt to instead be passed in your urine.”
“… a loop diuretic (water pill) that prevents your body from absorbing too much salt, allowing the salt to instead be passed in your urine.”
 AAKP is pleased to announce an opportunity for individuals with chronic kidney disease, and their caregivers, to participate in a research survey that will help us better understand the impact chronic kidney disease has had on their lives.
AAKP is pleased to announce an opportunity for individuals with chronic kidney disease, and their caregivers, to participate in a research survey that will help us better understand the impact chronic kidney disease has had on their lives. “I’d always thought that AKI and CKD were separate issues and I’ll bet you did, too. But Dr. L.S. Chawla and his co-writers based the following conclusion on the labor of epidemiologists and others. (Note: Dr. Chawla et al wrote a review article in the New England Journal of Medicine in 2014.)
“I’d always thought that AKI and CKD were separate issues and I’ll bet you did, too. But Dr. L.S. Chawla and his co-writers based the following conclusion on the labor of epidemiologists and others. (Note: Dr. Chawla et al wrote a review article in the New England Journal of Medicine in 2014.)
 One thing Dana asked that made me stop cold is “How do you cope with the inevitable aspects?” They are not inevitable, Dana. I am a lay person who has managed to keep my CKD at stage 3 for 11 years. I am also not a magician. What I am is someone who follows the guidelines for keeping my kidneys as healthy as possible.
One thing Dana asked that made me stop cold is “How do you cope with the inevitable aspects?” They are not inevitable, Dana. I am a lay person who has managed to keep my CKD at stage 3 for 11 years. I am also not a magician. What I am is someone who follows the guidelines for keeping my kidneys as healthy as possible.
 “A chronic inflammatory disease that is caused by autoimmunity. Patients with
“A chronic inflammatory disease that is caused by autoimmunity. Patients with 

 We all know diabetes raises your risk of developing Chronic Kidney Disease. But why? What’s the mechanism behind the fact? As far as I’m concerned, it’s time to find out.
We all know diabetes raises your risk of developing Chronic Kidney Disease. But why? What’s the mechanism behind the fact? As far as I’m concerned, it’s time to find out.
 good idea to limit red meat, and avoid processed meats.
good idea to limit red meat, and avoid processed meats.
 information about CKD. I was surprised to see a post seeming to claim that Human Immunodeficiency Virus (HIV) can cause CKD. How had I never heard about this before?
information about CKD. I was surprised to see a post seeming to claim that Human Immunodeficiency Virus (HIV) can cause CKD. How had I never heard about this before?



 Let’s finish out this lazy, hazy summer month of August with another reader question. This one was quite straight forward:
Let’s finish out this lazy, hazy summer month of August with another reader question. This one was quite straight forward:

 I come from a family of dancers. My parents and their siblings were all light on their feet and danced from the time they were teens right up until just before their deaths. It was a delight to watch them. The tradition continued with me… and my youngest who actually taught blues dancing for several years.
I come from a family of dancers. My parents and their siblings were all light on their feet and danced from the time they were teens right up until just before their deaths. It was a delight to watch them. The tradition continued with me… and my youngest who actually taught blues dancing for several years.
 HERE’S THE STORY
HERE’S THE STORY
 What does CKD research typically focus on?
What does CKD research typically focus on? 
 Let’s start at the beginning. FSGS is the acronym for focal segmental glomerulosclerosis. Anything look familiar? Maybe the ‘glomerul’ part of glomerulosclerosis? I think we need to know the definition of glomerulosclerosis to be able to answer that question. The National Institutes of Health’s U.S. National Library of Congress’s Medline Plus at
Let’s start at the beginning. FSGS is the acronym for focal segmental glomerulosclerosis. Anything look familiar? Maybe the ‘glomerul’ part of glomerulosclerosis? I think we need to know the definition of glomerulosclerosis to be able to answer that question. The National Institutes of Health’s U.S. National Library of Congress’s Medline Plus at 
 I think we need another definition here. Yep, it’s Plasmapheresis. Back to the Encarta Dictionary.
I think we need another definition here. Yep, it’s Plasmapheresis. Back to the Encarta Dictionary.
 Tubules, huh? What are those? Actually, the word just means tube shaped. Remembering that renal and kidney mean the same thing, we can see the problem area.
Tubules, huh? What are those? Actually, the word just means tube shaped. Remembering that renal and kidney mean the same thing, we can see the problem area.
 As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book,
As most of you know, I am extremely protective of my kidneys. When I was first diagnosed with Chronic Kidney Disease 11 years ago, my eGFR was only 39. Here’s a quick reminder of what the eGFR is from my first CKD book, 
 Ms. Rae-Garwood’s writing started out as a means to an end for a single parent with two children and a need for more income than her career as a NYC teacher afforded. Gail retired from both college teaching and acting – after a bit of soul searching about where her CKD limited energy would be best spent – early in 2013. Since her diagnose, Ms. Rae-Garwood writes most often about Chronic Kidney Disease, although she does write fiction. She has a three time award winning weekly blog (Surprise!) about this topic at
Ms. Rae-Garwood’s writing started out as a means to an end for a single parent with two children and a need for more income than her career as a NYC teacher afforded. Gail retired from both college teaching and acting – after a bit of soul searching about where her CKD limited energy would be best spent – early in 2013. Since her diagnose, Ms. Rae-Garwood writes most often about Chronic Kidney Disease, although she does write fiction. She has a three time award winning weekly blog (Surprise!) about this topic at 




 The blog has won several awards. Basically, that’s because I write in a reader friendly manner. After all, what good is all my researching if no one understands what I’m writing?
The blog has won several awards. Basically, that’s because I write in a reader friendly manner. After all, what good is all my researching if no one understands what I’m writing? National Kidney Month is just flying by. This is actually the last week and I doubt I’ll be able to post the rest of the 1in9 chapter before next month. But then again, it’s always Kidney Month for those of us with Chronic Kidney Disease. By the way, thank you to the reader who made it a point of telling me she can’t wait to read the rest of the chapter. Sooooo, let’s get started!
National Kidney Month is just flying by. This is actually the last week and I doubt I’ll be able to post the rest of the 1in9 chapter before next month. But then again, it’s always Kidney Month for those of us with Chronic Kidney Disease. By the way, thank you to the reader who made it a point of telling me she can’t wait to read the rest of the chapter. Sooooo, let’s get started!
 Exercise, something I loved until my arthritis got in the way, was also important. I was a dancer. Wasn’t that enough? Uh-uh, I had to learn about cardio and strength training exercise, too. It was no longer acceptable to be pleasantly plumb. My kidneys didn’t need the extra work. Hello to weights, walking, and a stationary bike. I think I took sleep for granted before CKD, too, and I now make it a point to get a good night’s sleep. A sleep apnea device improved my sleep—and my kidney function rose.
Exercise, something I loved until my arthritis got in the way, was also important. I was a dancer. Wasn’t that enough? Uh-uh, I had to learn about cardio and strength training exercise, too. It was no longer acceptable to be pleasantly plumb. My kidneys didn’t need the extra work. Hello to weights, walking, and a stationary bike. I think I took sleep for granted before CKD, too, and I now make it a point to get a good night’s sleep. A sleep apnea device improved my sleep—and my kidney function rose.
 While there are numerous objectives for this year’s World Kidney Day, the one that lays closest to my heart is this one: ‘Encourage systematic screening of all patients with diabetes and hypertension for CKD.’
While there are numerous objectives for this year’s World Kidney Day, the one that lays closest to my heart is this one: ‘Encourage systematic screening of all patients with diabetes and hypertension for CKD.’

 That, of course, prompted me to go directly to the National Kidney Foundation’s information about National Kidney Month at
That, of course, prompted me to go directly to the National Kidney Foundation’s information about National Kidney Month at  I wanted to share this quote from the AKF with you, both as a CKD awareness advocate and a woman:
I wanted to share this quote from the AKF with you, both as a CKD awareness advocate and a woman: health. However, the results of human studies are inconsistent…. To date, there have been two reported cases of a severe allergic reaction to dragon fruit.”
health. However, the results of human studies are inconsistent…. To date, there have been two reported cases of a severe allergic reaction to dragon fruit.” I have been researching for over two hours. I cannot find anything about atomic movement within the blood being measured by a blood pressure monitor of any kind. I’ve been to professional pages, checked studies, and even looked at advertisements. So, unless you have other information, I do believe I’ve been had. I just can’t wait to meet this young man at the follow up appointment in two weeks when I’ll ask him for resources and the monitor manufacturers’ information.
I have been researching for over two hours. I cannot find anything about atomic movement within the blood being measured by a blood pressure monitor of any kind. I’ve been to professional pages, checked studies, and even looked at advertisements. So, unless you have other information, I do believe I’ve been had. I just can’t wait to meet this young man at the follow up appointment in two weeks when I’ll ask him for resources and the monitor manufacturers’ information.
 Happy New Year! Here’s wishing you all a very healthy one. I, on the other hand, found myself in the cardiologist’s office the very first week of 2019. That was odd for me.
Happy New Year! Here’s wishing you all a very healthy one. I, on the other hand, found myself in the cardiologist’s office the very first week of 2019. That was odd for me.
 Busy with the holidays? Chanukah has passed, but we still have Christmas, Kwanzaa, and the New Year coming up. Feeling like you’re just too tired to deal with them? Maybe even fatigued? What’s the difference, you ask. Let’s go to Reuters at
Busy with the holidays? Chanukah has passed, but we still have Christmas, Kwanzaa, and the New Year coming up. Feeling like you’re just too tired to deal with them? Maybe even fatigued? What’s the difference, you ask. Let’s go to Reuters at  aldosterone and androgen hormones. The second part is the adrenal medulla, which creates noradrenaline and adrenaline.
aldosterone and androgen hormones. The second part is the adrenal medulla, which creates noradrenaline and adrenaline. “Blood Pressure
“Blood Pressure
 the symptoms. These are the same whether you’re the patient or the caretaker. I happen to be both a CKD patient and my Alzheimer’s husband’s caretaker, although we call me his care partner as suggested by the Alzheimer’s Association.
the symptoms. These are the same whether you’re the patient or the caretaker. I happen to be both a CKD patient and my Alzheimer’s husband’s caretaker, although we call me his care partner as suggested by the Alzheimer’s Association. Today is the last day of the eight day Chanukah celebration for us and all of you who celebrate this holiday. We usually throw a blowout party for anywhere from 30 to 50 people. But just a couple of months ago, we hosted a blowout pre-wedding potluck party for my daughter and her fiancé … and it was wonderful. Yet, it was clear that we can no longer handle undertaking such large parties. I had expressed my doubts last year about how long we’d be able to keep up the Chanukah party.
Today is the last day of the eight day Chanukah celebration for us and all of you who celebrate this holiday. We usually throw a blowout party for anywhere from 30 to 50 people. But just a couple of months ago, we hosted a blowout pre-wedding potluck party for my daughter and her fiancé … and it was wonderful. Yet, it was clear that we can no longer handle undertaking such large parties. I had expressed my doubts last year about how long we’d be able to keep up the Chanukah party.
 “Research shows that hearing loss is common in people with moderate Chronic Kidney Disease. As published in the American Journal of Kidney Diseases and highlighted on the
“Research shows that hearing loss is common in people with moderate Chronic Kidney Disease. As published in the American Journal of Kidney Diseases and highlighted on the 
 What should you do next? Based on your score, we recommend the following: A hearing test may be necessary to monitor your hearing loss. Now hearing loss is situational, and the next step you take is dependent on your need to hear in various listening situations. Some people can live with mild hearing losses. Others, such as teachers and therapists whose auditory skills are very important for their everyday work, require corrective technology — such as hearing aids — even when their hearing loss is at mild levels. It becomes important for them to do something about their hearing loss so they can function adequately in their work environment….
What should you do next? Based on your score, we recommend the following: A hearing test may be necessary to monitor your hearing loss. Now hearing loss is situational, and the next step you take is dependent on your need to hear in various listening situations. Some people can live with mild hearing losses. Others, such as teachers and therapists whose auditory skills are very important for their everyday work, require corrective technology — such as hearing aids — even when their hearing loss is at mild levels. It becomes important for them to do something about their hearing loss so they can function adequately in their work environment…. ask him not to, you say. Well, it’s involved. Basically, it’s because he has Alzheimer’s, doesn’t know how long winded he’s being, and feels terribly insulted when I ask him not to interrupt so I can write.
ask him not to, you say. Well, it’s involved. Basically, it’s because he has Alzheimer’s, doesn’t know how long winded he’s being, and feels terribly insulted when I ask him not to interrupt so I can write. energy. In Type 2 diabetes, either the pancreas does not make enough insulin or the body is unable to use insulin correctly.”
energy. In Type 2 diabetes, either the pancreas does not make enough insulin or the body is unable to use insulin correctly.” “Tau is one of two proteins—along with β-amyloid—that form unusual clumps in the brains of people with Alzheimer’s disease. Scientists have long debated which is most important to the condition and, thus, the best target for intervention. Tau deposits are found inside neurons, where they are thought to inhibit or kill them, whereas β-amyloid forms plaques outside brain cells.”
“Tau is one of two proteins—along with β-amyloid—that form unusual clumps in the brains of people with Alzheimer’s disease. Scientists have long debated which is most important to the condition and, thus, the best target for intervention. Tau deposits are found inside neurons, where they are thought to inhibit or kill them, whereas β-amyloid forms plaques outside brain cells.” By now it shouldn’t surprise me that as I’m out and about I’m constantly meeting more and more people with a connection to kidney disease. That was not the case 21 years ago, or even four years ago for that matter. What changed? The opening of my eyes to statistics I was previously unaware of, and frankly I found to be quite shocking and unacceptable. I’ll get to those stats a little later.
By now it shouldn’t surprise me that as I’m out and about I’m constantly meeting more and more people with a connection to kidney disease. That was not the case 21 years ago, or even four years ago for that matter. What changed? The opening of my eyes to statistics I was previously unaware of, and frankly I found to be quite shocking and unacceptable. I’ll get to those stats a little later.
 kidneys failed! He and his dance partner and instructor, Brianna Santiago, spent six months of grueling practices preparing for their energetic performance to Pharrell William’s song Happy, demonstrating the improved quality of life home dialysis can provide, and that dialysis does not have to be a death sentence.
kidneys failed! He and his dance partner and instructor, Brianna Santiago, spent six months of grueling practices preparing for their energetic performance to Pharrell William’s song Happy, demonstrating the improved quality of life home dialysis can provide, and that dialysis does not have to be a death sentence. University of Arizona
University of Arizona  Hmmm, maybe that title should read “Famous People Who Died from Kidney Disease.” Let’s go back a bit to see what I’m talking about. By now you know my youngest married on the 6th of this month. Thank you to everyone who sent their best wishes. She and her husband did a wonderful job of creating the wedding they wanted, just as the new Mr. & Mrs. Nielson are doing a terrific job of creating the life they want together.
Hmmm, maybe that title should read “Famous People Who Died from Kidney Disease.” Let’s go back a bit to see what I’m talking about. By now you know my youngest married on the 6th of this month. Thank you to everyone who sent their best wishes. She and her husband did a wonderful job of creating the wedding they wanted, just as the new Mr. & Mrs. Nielson are doing a terrific job of creating the life they want together.
 Keep those years in mind. Keep in mind also that there was no dialysis or transplantation when these people died of kidney disease.
Keep those years in mind. Keep in mind also that there was no dialysis or transplantation when these people died of kidney disease.
 Food and Drug Administration
Food and Drug Administration

 You’d think that leaves me out, but you’d be wrong. I’m writing for pre-menopausal women…and for anyone who wants to know what menstrual cycles have to do with Chronic Kidney Disease. I’m one of those who wants to know.
You’d think that leaves me out, but you’d be wrong. I’m writing for pre-menopausal women…and for anyone who wants to know what menstrual cycles have to do with Chronic Kidney Disease. I’m one of those who wants to know.
 Whoa! I wouldn’t want even more of these substances in my body. Not only would they make the CKD worse, but also its effects on my body. According to Medical News Today at
Whoa! I wouldn’t want even more of these substances in my body. Not only would they make the CKD worse, but also its effects on my body. According to Medical News Today at 


 In some ways, I live the typical middle class American mom life. I have a middle schooler and a high schooler. I work from home, my husband works a 9-5 in an office. The kids go to school, do their homework, go to activities. I have coffee dates with friends and dinner out with family, we go to the movies, we stay home and do yard work. Same routine, same rhythm as so many other families we know.
In some ways, I live the typical middle class American mom life. I have a middle schooler and a high schooler. I work from home, my husband works a 9-5 in an office. The kids go to school, do their homework, go to activities. I have coffee dates with friends and dinner out with family, we go to the movies, we stay home and do yard work. Same routine, same rhythm as so many other families we know.




 is primarily set in Brooklyn.” Hmmm, two appealing actors AND it was set in Brooklyn. I still wasn’t sure so I emailed back asking if SlowItDownCKD was the intended recipient for this email. Once assured it was, I agreed. Hey, I’m always up for an adventure.
is primarily set in Brooklyn.” Hmmm, two appealing actors AND it was set in Brooklyn. I still wasn’t sure so I emailed back asking if SlowItDownCKD was the intended recipient for this email. Once assured it was, I agreed. Hey, I’m always up for an adventure.

 “Scientists estimate that kidney dysplasia affects about one in 4,000 babies…. This estimate may be low because some people with kidney dysplasia are never diagnosed with the condition.”
“Scientists estimate that kidney dysplasia affects about one in 4,000 babies…. This estimate may be low because some people with kidney dysplasia are never diagnosed with the condition.”
 AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”
AAKP has grown into a nationally recognized patient organization that reaches over 1 million people yearly. It remains dedicated to providing patients with the education and knowledge necessary to ensure quality of life and quality of health.”
 The first thing the American Society of Nephrology requested is that those of you who are familiar with Twitter, or are willing to become familiar with this social media, join the monthly #AskASN twitter chats. To join Twitter you simply go to Twitter.com and sign yourself up, no special expertise necessary. That pound sign, or as it’s commonly known now – hashtag, before the words signify that this is a person or group with a Twitter account. What comes after the hashtag is your handle, the name you choose for yourself. Mine is – naturally – #SlowItDownCKD. You can search for me on Twitter.
The first thing the American Society of Nephrology requested is that those of you who are familiar with Twitter, or are willing to become familiar with this social media, join the monthly #AskASN twitter chats. To join Twitter you simply go to Twitter.com and sign yourself up, no special expertise necessary. That pound sign, or as it’s commonly known now – hashtag, before the words signify that this is a person or group with a Twitter account. What comes after the hashtag is your handle, the name you choose for yourself. Mine is – naturally – #SlowItDownCKD. You can search for me on Twitter.
 Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at
Oh, wait. First we need to know what a webinar is. My favorite online dictionary, Merriam-Webster, at 
 That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible.
That means it has all the content, but I didn’t like the formatting so I re-did it. Would you like it? If so, just be the first one to contact me to let me know. Oh, one restriction: only those who haven’t received a free book from me before, please. I’d like to share the CKD information with as many people as possible.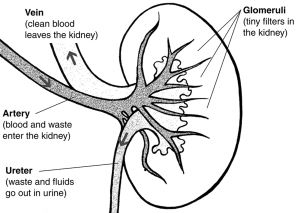 A typical kidney is the size of a human fist and weighs about a third of a pound. PKD kidneys can be much larger, some growing as large as a football, and weighing up to 30 pounds each. The number of cysts can range from just a few to many. The size of the cysts can range from a pinhead to as large as a grapefruit. Although the primary sign of PKD is cysts in the kidneys, there are other symptoms that can occur in various areas of the body.”
A typical kidney is the size of a human fist and weighs about a third of a pound. PKD kidneys can be much larger, some growing as large as a football, and weighing up to 30 pounds each. The number of cysts can range from just a few to many. The size of the cysts can range from a pinhead to as large as a grapefruit. Although the primary sign of PKD is cysts in the kidneys, there are other symptoms that can occur in various areas of the body.”
 Let’s see if I can find something more recent. This, from the National Kidney Fund at
Let’s see if I can find something more recent. This, from the National Kidney Fund at 
 When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
When I was a little girl, I liked to listen to my father whistle ‘All of Me,’ written by Marks and Simon in 1931 when Charlie, my father, was just 16. Only a few years later, it became a sort of love language for my mother and him. Enter a former husband of my own and my children. When my folks visited from Florida and my then husband’s side of the family journeyed over to Staten Island from Brooklyn to visit them, they all sang the song with great emotion. (By then, Bell’s palsy had robbed my father of the ability to whistle.)
 Better Information
Better Information

 “Then I found this in BrightHub.com’s February 13th article The Importance of the Potassium and Sodium Balance.
“Then I found this in BrightHub.com’s February 13th article The Importance of the Potassium and Sodium Balance. Will she need extra medicines when she’s pregnant? Women trying to get pregnant should start taking the vitamin folic acid to reduce the chance of their baby having spina bifida, an abnormality of the spinal cord. The normal dose of folic acid is 400ug per day and can be bought over the counter. However, if the folate level is low or a patient is on the drug azathioprine which affects the way folic acid works, the dose of 5mg daily may be prescribed. No other over the counter vitamins are required unless specifically advised by a doctor or midwife. All pregnant patients should avoid additional supplements of vitamin A. If vitamin D levels are low GPs will advise correction with high dose prescribed vitamin D (also known as cholecalciferol). Women with kidney diseases are at higher risk of pre-eclampsia. Aspirin lowers the risk of pre eclampsia, and women with CKD are usually offered a low dose aspirin (75mg once daily) throughout pregnancy unless there are specific reasons not to take it e.g. they are allergic to aspirin. Pregnant women with a high level of protein in their urine have an increased risk of developing blood clots (thrombosis). This can be reduced by small daily injections of low molecular weight heparin. Heparin reduces the way the blood clots. Both pregnancy and CKD can cause a low blood count (
Will she need extra medicines when she’s pregnant? Women trying to get pregnant should start taking the vitamin folic acid to reduce the chance of their baby having spina bifida, an abnormality of the spinal cord. The normal dose of folic acid is 400ug per day and can be bought over the counter. However, if the folate level is low or a patient is on the drug azathioprine which affects the way folic acid works, the dose of 5mg daily may be prescribed. No other over the counter vitamins are required unless specifically advised by a doctor or midwife. All pregnant patients should avoid additional supplements of vitamin A. If vitamin D levels are low GPs will advise correction with high dose prescribed vitamin D (also known as cholecalciferol). Women with kidney diseases are at higher risk of pre-eclampsia. Aspirin lowers the risk of pre eclampsia, and women with CKD are usually offered a low dose aspirin (75mg once daily) throughout pregnancy unless there are specific reasons not to take it e.g. they are allergic to aspirin. Pregnant women with a high level of protein in their urine have an increased risk of developing blood clots (thrombosis). This can be reduced by small daily injections of low molecular weight heparin. Heparin reduces the way the blood clots. Both pregnancy and CKD can cause a low blood count ( But then I wondered why I’ve been taking it all these years since I don’t have cardiology problems. Hmmm, I do have osteoarthritis and can’t take NSAIDS. In
But then I wondered why I’ve been taking it all these years since I don’t have cardiology problems. Hmmm, I do have osteoarthritis and can’t take NSAIDS. In  function of inflammation is to eliminate the initial cause of cell injury, clear out necrotic cells and tissues damaged from the original insult and the inflammatory process, and initiate tissue repair.”
function of inflammation is to eliminate the initial cause of cell injury, clear out necrotic cells and tissues damaged from the original insult and the inflammatory process, and initiate tissue repair.”
 male or female or of varying socioeconomic status; however the happiest participants had the best results across the board for the health markers. I.e. happier people had lower heart rates, and an average of 32% lower levels of cortisol which can have a direct effect on other elements such as blood sugar.”
male or female or of varying socioeconomic status; however the happiest participants had the best results across the board for the health markers. I.e. happier people had lower heart rates, and an average of 32% lower levels of cortisol which can have a direct effect on other elements such as blood sugar.” Want a little reminder about metabolism? I do. According to Dr. Ananya Mandal from News Medical Life Sciences at
Want a little reminder about metabolism? I do. According to Dr. Ananya Mandal from News Medical Life Sciences at 
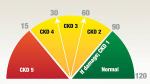 decline in our kidney function. I maintain that if only my primary care physician had told me when he first noticed that 39% GFR, maybe I wouldn’t be in stage 3 of 5. Maybe those now on dialysis or searching for a transplant wouldn’t be in the position they are, either.
decline in our kidney function. I maintain that if only my primary care physician had told me when he first noticed that 39% GFR, maybe I wouldn’t be in stage 3 of 5. Maybe those now on dialysis or searching for a transplant wouldn’t be in the position they are, either.
 The literature suggests early nephrologist involvement improves long-term outcomes. Proactive primary care offers longitudinal guidance for making the enormous lifestyle changes in diet, exercise, stress management, hydration, sleep and toxic exposures, while offering psychological counseling that is required to achieve such changes. The cross-over benefits for patients’ other diagnoses is well known.
The literature suggests early nephrologist involvement improves long-term outcomes. Proactive primary care offers longitudinal guidance for making the enormous lifestyle changes in diet, exercise, stress management, hydration, sleep and toxic exposures, while offering psychological counseling that is required to achieve such changes. The cross-over benefits for patients’ other diagnoses is well known. surgeries, travel and stress — need to grasp a breadth of nephrology basics. Our patients with CKD are at increased risk of acute kidney injury. Astute protection means we save nephrons. This author would welcome renal rotations at all levels of medical training, with a facet of focus on longitudinal outpatient, early and moderate CKD care. This vision of collaboration, with a commitment to early diagnosis and intervention, offers the opportunity to learn how to guide patients to a less inflammatory lifestyle.
surgeries, travel and stress — need to grasp a breadth of nephrology basics. Our patients with CKD are at increased risk of acute kidney injury. Astute protection means we save nephrons. This author would welcome renal rotations at all levels of medical training, with a facet of focus on longitudinal outpatient, early and moderate CKD care. This vision of collaboration, with a commitment to early diagnosis and intervention, offers the opportunity to learn how to guide patients to a less inflammatory lifestyle.

