We have a habit of using the dining room table as our desks when we both want to work yet be together while doing so. But it is our dining room table. That means each time we have company over for dinner, we need to clear the table. Bear brings his papers into his office, and I bring mine into my office. I’ve really slowed down since the pancreatic cancer, so sometimes papers are piled upon the papers I haven’t yet organized from the last time we had dinner guests.

Here in the USA, last weekend was Mother’s Day. Hello to my lovely daughter, her husband, and the two little boys. And there goes another bunch of papers into my office. This is not my usual way. I like neat. I like organized. I couldn’t stand it anymore so I started cleaning them up. At the very bottom of one pile, I found the word ‘angiomyolipoma’ on a piece of scrap paper. That was it, nothing other than that word. Of course, I just had to know what it meant [which might have given me a clue as to why it was there on my desk at all].
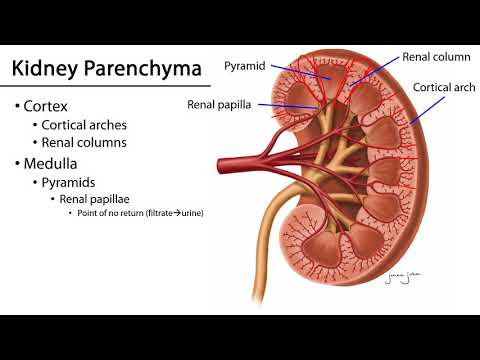
I discovered that it’s also called ‘renal angiomyolipoma.’ Aha! Renal, that means kidney. Of course, I needed to know more so I turned to The Cleveland Clinic.
“A renal angiomyolipoma (AML) is a type of tumor in your kidney. Almost all are benign (noncancerous), but they can hemorrhage, which can be life-threatening. A tumor occurs when cells grow and divide more than they should. A renal angiomyolipoma is made of blood vessels, muscle cells and fat.”
Why would that happen, I wondered. Turns out I wasn’t the only one wondering. After perusing many sites, I realized no one knew what really caused renal angiomyolipoma. However, the American Hospital in Paris offered the following as possible causes:
- “ Tuberous sclerosis (TS), also known as Bourneville disease: a rare genetic disease that stimulates the development of angiomyolipomas. Patients with TS frequently present with multiple angiomyolipomas affecting both kidneys.
- Associated genetic syndromes: Angiomyolipomas may be linked to other genetic diseases, such as Cowden syndrome.
- Feminine gender: statistics show that women are more likely than men to develop angiomyolipomas. This increased prevalence in women suggests that hormones may influence the growth of these tumors.”
Maybe I’ll do better looking for the symptoms. Bingo! VerywellHealth offers the following:
“It is common to have an angiomyolipoma without any symptoms. More than 80% of these tumors are found by chance during imaging tests for other issues….
Though rare, symptoms typically occur when the tumor grows to 40 millimeters (mm) (a little over 1.5 inches) or larger and begins to spread. In tumors of this size, symptoms can occur in 80% of cases and can include the following…:

- Flank pain (pain between your back and abdomen on one or both sides of your body)
- A palpable mass (a mass that can be felt)
- Hematuria (blood in your urine)
- Newly diagnosed high blood pressure
- Anemia
- Urinary tract infection (UTI)
- Renal (kidney) failure
A 40 mm or larger angiomyolipoma can cause spontaneous retroperitoneal hemorrhage, also called Wunderlich syndrome. This rare but potentially life-threatening condition involves bleeding in the area behind your abdominal cavity. It affects fewer than 15% of people who have these tumors….”
I wonder if there’s any connection between the fact that chronic kidney disease often has no symptoms and now we find that is also true of renal angiomyolipoma? But that’s a blog for another day.
What about diagnosis? How is that made? According to MedicineNet:
“The preliminary diagnosis of angiomyolipoma is usually done either incidentally while the patient is undergoing imaging tests for other reasons or directly by ultrasound, CT scan, and/or MRI scan. Urologists, radiologists, and emergency medicine physicians are often the first doctors to suspect and/or diagnose these tumors. In addition, ob-gyn doctors may find such tumors while doing ultrasound studies on pregnant females; angiomyolipoma bleeding problems are rare but possible in pregnancy.”
Let’s see now. We’ve looked at what it is, what may cause it, what the symptoms may be, and diagnosis. What’s next? Of course, it’s the treatment. Hmmm, time to check MedicalNewsToday:
“In some cases, particularly when the angiomyolipoma causes symptoms, a doctor may suggest the following:
- Selective renal artery embolization: A minimally invasive procedure that involves inserting a catheter through an artery into the leg and guiding it to the renal arteries. The surgeon then injects particles into the blood vessels around the tumor, blocking its blood flow and reducing its size.
- Nephron-sparing surgery: This procedure removes the tumor while preserving as much kidney tissue as possible.
- Complete nephrectomy: This is a type of surgery that removes the entire kidney.
- Ablation: Some methods include cryoablation and radiofrequency techniques. These procedures involve using extreme cold or heat to destroy tumor tissue.
- Treatment with mTOR inhibitors: These medications may help individuals with TSC manage their angiomyolipomas.”

Time to switch topics. I’d promised Elizabeth Oldham I’d let you know about the Cleveland Asian Festival only to find out it was this past weekend. Why not keep your eyes on her Facebook page to see what other kidney related festivals she’s volunteering at? Sorry, Elizabeth. BUT, here’s the next occasion Elizabeth has posted:
“Calling All Wellness Warriors!
Are you ready to level up your health game? Join us at the Cleveland MOTTEP Workshop:
“How to Be a Wellness Warrior” and unlock the secrets to vibrant living!
Join us June 29th, 2024 at Centers for Dialysis Care East from 10am-1pm. Secure Your Spot:
Visit our website at (https://clevelandmottep.org) or dial 216-658-0727 to RSVP. Limited spots available—don’t miss out!
All participants will receive a gift card after completing the workshop!”
Hopefully those of you in Cleveland, Ohio, will be able to save that date.
Until next week,
Keep living your life!