What a whirlwind week it’s been here in Arizona. We’ve taken the Red Rock Jeep Tour in Sedona, lunched at The Asylum in Jerome, and visited The Palace Restaurant and The Sharlott Hall Museum in Jerome, all while we stayed in The Vendome Hotel in Prescott. We’ve even been to Arizona Broadway Theater for lunchtime theater and to Sustainable Blues for a dance lesson. No wonder my brother and sister-in-law had to go home to get some rest.
for a dance lesson. No wonder my brother and sister-in-law had to go home to get some rest.
The only thing consistent about this past week, like every week since I’ve been diagnosed with Chronic Kidney Disease is no kidney pain. Yet, a reader has told me she experiences pain in her kidneys although her doctors tell her this is not a symptom of kidney disease. Unfortunately, I neglected to ask what kind of kidney disease she has when I offered to blog about this for her.
When I started researching, I found there are many different causes for kidney pain. MedicineNet.com at http://www.medicinenet.com/kidney_pain/page3.htm offers a list of these causes:
“Some of the major underlying causes of kidney pain or flank pain are as follows:
- Urinary tract infections, mainly pyelonephritis
- Kidney stones
- Diabetes
- Glomerulonephritis
- High blood pressure
- Polycystic kidney disease (congenital)
- Congenital malformations in the renal system resulting in complete or partial blockage of urine flow
 Drugs or toxins that harm kidney tissue (for example, pesticide exposure or chronic use of medications such as ibuprofen [Advil, Motrin, and others])
Drugs or toxins that harm kidney tissue (for example, pesticide exposure or chronic use of medications such as ibuprofen [Advil, Motrin, and others])- Drinking alcohol may cause acute or chronic flank pain; the pain source, depending on the individual, may be from the kidneys or the liver.”
Wow! And doctors say kidney pain is not a symptom of CKD? Notice the two leading causes of CKD on this list: diabetes and high blood pressure. Oh, and the “drugs or toxins that harm kidney tissue….”
I clearly remember being asked if I had flank pain when I was first diagnosed… and I clearly remember asking where the flank was. For those of you like me who don’t know, the primary definition of flank is “the fleshy part of the side between the ribs and the hip.” Thank you for that Merriam Webster Dictionary at http://www.merriam-webster.com/dictionary/flank.
Then, never having experienced it myself, I had to know what it felt like – or at least find a description of the pain. eHealthStar (which is a new site for me) at http://www.ehealthstar.com/what-does-kidney-pain-feel-like.php describes it as:
- Sudden (acute) or persistent (chronic)
- Mild or severe
- Sharp, dull, throbbing or, rarely, cramping or colicky
- One sided or both-sided.
Kidney pain is often, but not always, associated with tenderness in the kidney area.
Wait a minute; that’s covers just about every kind of pain you can think of. So if you have a pain in your flank area, you have CKD – right?
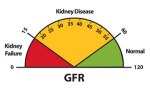
Wrong. Remember the list of other possible causes. We’re familiar with kidney stones – a crystallization of mineral and acid salts that form a stone in the kidneys – which are not CKD. The ‘C’ in CKD is for chronic or long term, in this case long term deterioration of your kidney function.
Drinking, while it may affect CKD, is not CKD. If you drink and experience flank pain, it does not mean you have CKD nor that you’re going to develop CKD. Although, it might not be a bad idea to be tested should you have your suspicions. Speak to your primary care doctor about this.
Numerous urinary tract infections may be a cause of CKD, but a single urinary tract infection may not. Even if you’ve had numerous UTIs, this does not mean that the pain from these indicates CKD. Although….
Pyelonephritis, an infection of the kidneys is a more serious UTI, as explained by WebMD at http://www.webmd.com/a-to-z-guides/kidney-infections-symptoms-and-treatments
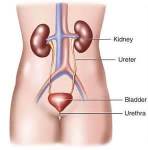
“Most cases of pyelonephritis are complications of common bladder infections. Bacteria enter the body from the skin around the urethra. They then travel up the urethra to the bladder.
Sometimes, bacteria escape the bladder and urethra, traveling up the ureters to one or both kidneys.
Pyelonephritis is a potentially serious kidney infection that can spread to the blood, causing severe illness. Fortunately, pyelonephritis is almost always curable with antibiotics.”
This makes quite a bit of sense. The second nephrologist to treat me referred me to an urologist when he realized I was on my fifth UTI in the same summer and he suspected this one had spread to my bladder.
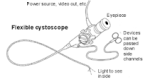 The urologist actually had me look through the cystoscope myself to reassure me that the lower urinary tract infection had not spread to the upper urinary tract where the bladder is located. Believe me, it felt surreal to be able to look inside my own body in real time.
The urologist actually had me look through the cystoscope myself to reassure me that the lower urinary tract infection had not spread to the upper urinary tract where the bladder is located. Believe me, it felt surreal to be able to look inside my own body in real time.
Notice I’m exploring all the items on the list although not in the order MedicineNet.com offers them.
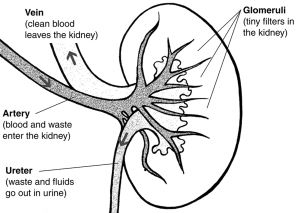
What’s next? Let’s take a look at Glomerulonephritis. I went right back to my old friend The Mayo Clinic at http://www.mayoclinic.org/diseases-conditions/glomerulonephritis/basics/definition/con-20024691 for some answers. That’s where I found this definition of the disease:
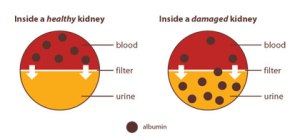
“Glomerulonephritis (gloe-mer-u-low-nuh-FRY-tis) is inflammation of the tiny filters in your kidneys (glomeruli). Glomeruli remove excess fluid, electrolytes and waste from your bloodstream and pass them into your urine. Also called glomerular disease, glomerulonephritis can be acute — a sudden attack of inflammation — or chronic — coming on gradually.”
So this one does have more to do with the kidneys, but it’s still not CKD. It can be acute, which CHRONIC kidney disease cannot. Obviously, congenital diseases or malfunctions of the kidney are also not CKD since you are born with them, rather than having a slow deterioration of your kidney function.
For the life of me (cute, huh?), I cannot understand why a nephrologist would tell a CKD patient that flank – or kidney – pain cannot be associated with CKD when this may be one of the symptoms. I’m going to have to suggest to the reader that asked for this blog that she challenge her nephrologist… again.
 Want to hear about What Is It and How Did I Get It? Early Stage Chronic Kidney Disease? Of course, you do (she decided unilaterally). I was delighted to have new blog readers inform me that they’ve ordered multiple copies of the book for friends and family since these same new readers are also newly diagnosed CKD patients. Hurray! Some people are taking my advice.
Want to hear about What Is It and How Did I Get It? Early Stage Chronic Kidney Disease? Of course, you do (she decided unilaterally). I was delighted to have new blog readers inform me that they’ve ordered multiple copies of the book for friends and family since these same new readers are also newly diagnosed CKD patients. Hurray! Some people are taking my advice.
Until next week,
Keep living your life.



 “During the deep stages of NREM sleep, the body repairs and regenerates tissues, builds
“During the deep stages of NREM sleep, the body repairs and regenerates tissues, builds