Our old friend, Leesa Thompson …. Wait a minute! I don’t mean you’re old, Leesa. I mean we’ve had a couple of guest blogs from you before. Please forgive me. Anyway, Leesa has brought another guest blog to me. This one is perfect for National Kidney Month and a lovely way to end this celebratory month. Take it away, Leesa…
National Kidney Month is observed annually in March to raise awareness about kidney health, kidney disease prevention, and the importance of early detection and treatment. During this month-long observance, various organizations, including the National Kidney Foundation (NKF) and the American Kidney Fund (AKF), as well as healthcare providers and advocates, work to educate the public about kidney health and the risk factors associated with kidney disease. The primary goals of National Kidney Month are to:
1. Raise Awareness: National Kidney Month aims to increase awareness about the importance of kidney health and the prevalence of kidney disease, which affects millions of people worldwide. By educating the public about the risk factors, symptoms, and complications of kidney disease, advocates hope to encourage individuals to take proactive steps to protect their kidney health.
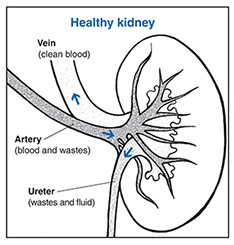
2. Promote Prevention: Kidney disease is often preventable or manageable when detected early. National Kidney Month provides an opportunity to promote healthy lifestyle habits, such as maintaining a balanced diet, staying hydrated, exercising regularly, managing blood pressure and blood sugar levels, and avoiding tobacco use, which can help reduce the risk of developing kidney disease.
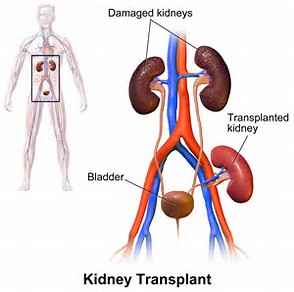
3. Support Patients: National Kidney Month also serves as a platform to show support for individuals living with kidney disease and those who have undergone kidney transplantation. It highlights the importance of access to quality healthcare, treatment options, and support services for kidney disease patients and their families. Throughout National Kidney Month, activities may include educational events, screenings, fundraisers, advocacy campaigns, and social media initiatives aimed at raising awareness and promoting kidney health. By participating in these activities and spreading the word about kidney health, individuals can help reduce the burden of kidney disease and improve outcomes for those affected by this condition.

Donate Life Month is an observance held annually in April [Gail here: more on that next month] to raise awareness about organ donation and encourage individuals to register as organ, eye, and tissue donors. During Donate Life Month, various events, campaigns, and educational initiatives are organized by organizations such as Donate Life America, transplant centers, and other healthcare organizations to promote the importance of organ donation and transplantation. The primary goal of Donate Life Month is to inspire people to make the decision to become organ donors and to discuss their wishes with their families. By increasing awareness about the critical need for organ donors and dispelling myths and misconceptions surrounding donation, advocates hope to save more lives and improve the quality of life for individuals awaiting life-saving transplants. Throughout the month of April, activities may include community outreach events, educational workshops, social media campaigns, donor registration drives, and storytelling initiatives featuring transplant recipients, donor families, and healthcare professionals. These efforts aim to highlight the profound impact of organ donation on individuals and communities and to encourage meaningful conversations about donation and transplantation. Participation in Donate Life Month provides an opportunity for individuals to learn more about the donation process, the importance of registering as a donor, and the incredible gift of life that organ donation represents. By engaging with the Donate Life community and supporting initiatives to raise awareness, individuals can help to increase the number of registered donors and ultimately save more lives through organ transplantation.
Becoming a living kidney donor is a decision that carries significant weight, both for the donor and the recipient. Understanding the full spectrum of advantages and disadvantages associated with this altruistic act is essential for individuals contemplating such a profound gesture, particularly in light of the critical shortage of available kidneys for transplantation.

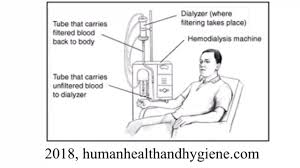
On the positive side, the primary benefit of being a living kidney donor lies in the opportunity to save a life. With approximately 100,000 individuals approved for kidney transplants in the United States alone, the demand for organ donors far exceeds the available supply. By offering one of their kidneys to someone suffering from kidney failure, donors directly impact the recipient’s health and lifespan. This act of selflessness not only saves a life but also brings immeasurable satisfaction and a deep sense of fulfillment to the donor, knowing they’ve made a tangible and potentially life-saving difference in another person’s life. Moreover, the impact of a kidney donation extends beyond the individual recipient to their family, friends, and community. It fosters a culture of compassion and generosity, inspiring others to consider organ donation as a means of giving back and making a positive impact on society. Additionally, undergoing the rigorous medical evaluation process before donation can lead to early detection and treatment of previously undiagnosed health issues in the donor, ensuring the best possible outcome for both parties involved. Furthermore, living kidney donors typically experience minimal long-term health effects, with studies indicating that they generally enjoy good health and life expectancy post-donation. This reassurance can alleviate concerns about the potential impact on the donor’s own health and well-being. Additionally, the experience of being a living kidney donor can lead to personal growth and a deeper appreciation for one’s own health. Donors often report feeling a renewed sense of purpose and gratitude for their own well-being, inspiring them to prioritize self-care and adopt healthier lifestyle habits.
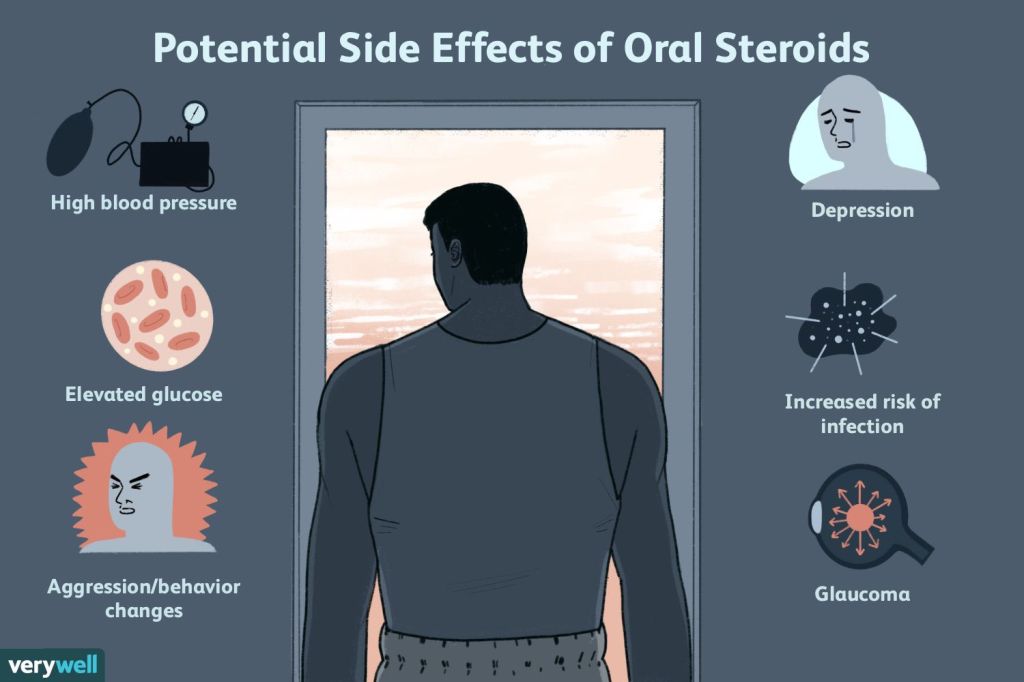
However, despite the numerous benefits associated with being a living kidney donor, there are also potential drawbacks and considerations to be mindful of. Donating a kidney involves undergoing surgery, which carries inherent risks such as bleeding, infection, and adverse reactions to anesthesia. While serious complications are rare, donors must be prepared for the physical discomfort and recovery period following surgery, which may necessitate several weeks of rest and limited activity. Furthermore, the emotional and psychological impact of being a living kidney donor should not be underestimated. Donors may experience a range of emotions, including anxiety, guilt, and worry about the recipient’s well-being, as well as concerns about their own health and future. It is essential for donors to have access to adequate support and counseling throughout the donation process to address any emotional challenges and ensure their well-being. Additionally, there may be practical and logistical considerations to contend with, such as arranging time off from work for surgery and recovery, coordinating travel and accommodations if the donor and recipient are not in the same location, and navigating financial expenses related to the donation process. Donors should carefully plan and prepare for these logistical challenges to minimize stress and ensure a smooth donation experience.
In summary, while being a living kidney donor offers the opportunity to save a life and make a profound difference in someone’s life, it is essential for individuals to carefully weigh the potential risks and benefits before making this decision. By thoroughly considering all aspects of the donation process and seeking support from medical professionals and support networks, potential donors can make an informed decision that aligns with their values and priorities, ultimately contributing to the greater good and leaving a lasting legacy of compassion and generosity.
Thank you for closing out National Kidney Month and easing us into National Donate Life Month, Leesa.
Until next week,
Keep living your life!